- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Man develops severe liver damage after Epsom salt naturopathy
A 38-year-old man developed serious liver damage after taking epsom salts to treat gallstones, reveal doctors in the journal BMJ Case Reports.
The patient a non-alcoholic, non-diabetic man with gallstone disease was prescribed three tablespoons of Epsom salt (magnesium sulfate crystals) with lukewarm water for 15 days for ‘stone dissolution’ by a naturopathy practitioner. He developed loss of appetite and darkening of urine from the 12th day on treatment and jaundice from the second day after treatment completion. The patient denied fevers, skin rash, joint pains, myalgia, abdominal pain, abdominal distension and cholestatic symptoms.
Examination revealed a deeply icteric patient oriented to time, place and person without organomegaly or stigmata of chronic liver disease. Blood investigations revealed platelet count 190 (normal 150–450 x 109/L), total bilirubin 12.8 (39.3 mmol/L) (normal 0.3–1.0 mg/dL or 5.0–17.0 mmol/L), direct bilirubin 6.9 (21.7 mmol/L) (0.0–0.2 mg/dL or 0.0–3.4 mmol/L), aspartate aminotransferase 508 (<37 U/L), alanine aminotransferase 228 (<41 U/L), γ-glutamyltransferase 298 (5–61 U/L), alkaline phosphatase 178 (35–129 U/L), albumin 4.2 (3.5–5.0 g/dL) and international normalised ratio 1.1 (0.9–1.2). R ratio was 3.84 and Roussel Uclaf Causality Assessment Method score was 8 (probable adverse drug reaction). Serum magnesium was 3.1 (1.7–2.4 mg/dL). Tests for viral hepatitis A, E, B, C, cytomegalovirus, Epstein-Barr and herpes simplex viruses and those for autoimmune hepatitis and IgG4 disease were unremarkable.
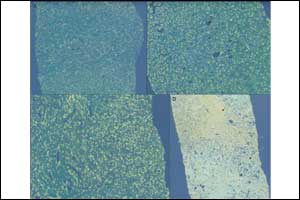
There was no evidence of underlying sepsis and other organ failures. Contrast enhanced CT of upper abdomen revealed only hepatomegaly with mild periportal oedema. Percutaneous liver biopsy revealed submassive necrosis with dense portal-based fibrosis, mixed portal inflammation, extensive perivenular canalicular and hepatocellular cholestasis with macrovesicular steatosis and perisinusoidal fibrosis (suggestive of steatohepatitis) without evidence of granulomas, inclusion bodies or vascular changes suggestive of acute drug-induced liver injury . Polarising microscopy did not reveal crystalline deposits. Drug withdrawal and adequate hydration were instated and the patient had an uneventful recovery with normalisation of liver function tests after 38 days. Common adverse effects of Epsom salt overuse include diarrhoea, dyselectrolytaemia, renal injury and cardiac arrhythmias.
Liu et al described the patterns of mineral-associated hepatic injury due to inhalational or intravenous exposure with pure silica, chromium-cobalt alloy and magnesium silicate (talc) in seven patients. They demonstrated that silica led to formation of sclerohyaline nodules within portal tracts and lobules in contrast to magnesium silicate injury that was associated with a predominant reactive fibrosis in portal and centrilobular areas. These patients were chronically exposed, in contrast to our patient who consumed Epsom salt in large quantities within a short period of time leading to predominantly necrotic and dense reactive fibrotic type of injury. Epsom salt-related severe liver injury and its histopathology have not been described in literature before. The Roussel Uclaf Causality Assessment Method (RUCAM) score was strongly suggestive of Epsom salt injury in our patient. We believe that underlying non-alcoholic steatohepatitis potentiated extensive liver injury in our patient, which resolved on stopping the offending agent.
Carry home points :
Epsom salt intake could lead to severe injury in predisposed patients.
Non-alcoholic fatty liver disease or steatohepatitis could act as a potential risk factor for development of magnesium sulfate liver injury.
Oral magnesium salt-related liver injury has a predominant dense portal-based expansile reactive fibrosis and associated necrosis with mixed cellular inflammation.
For more details click on the link: doi:10.1136/bcr-2017-221718

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd