- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Lung Abscess - Standard Treatment Guidelines
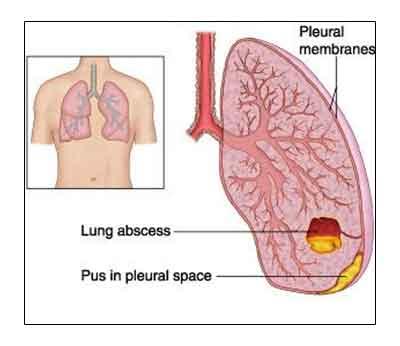
Lung abscess is a common form of suppurative lung disease that is characterized by a localized necrosis of pulmonary parenchyma and circumscribed collection of pus in the lung that is usually greater than 2 cm in diameter. Many local causes and systemic diseases can result in lung abscess formation. Primary lung abscess is more common and develops as a result of necrosis of lung parenchyma due to an existing disease process that is occurring there, such as, untreated aspiration pneumonia especially due to staphylococcal klebsiella and anaerobic organisms,, or lung cancer. A lung abscess can also develop secondary to preexisting conditions, such as, bronchial obstruction, spread from an extrapulmonary focus of infection, bronchiectasis, or immunocompromised state. Acute and chronic is based on duration; acute <6 weeks and chronic > 6 weeks
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Lung Abscess. Following are the major recommendations :
Case definition:
(For both situations of care)
Primary lung abscess
- A patient with an ongoing episode of pneumonia of 2 to 3 weeks duration, or, a history of pneumonia in the recent past presents with respiratory symptoms and signs consistent with a lung abscess, (such as, cough, sputum, that may be putrid and foul smelling, haemoptysis, pleuritic chest pain, shoulder pain, or heaviness in the chest) and systemic manifestations like fever, night sweats, anorexia, weight loss, and digital clubbing.
- Chest radiograph evidence of a cavity or cavities with a fluid level
Incidence of The Condition In India
Globally, the incidence of lung abscess has declined by nearly 10-fold during the preceding few decades in comparison with the pre-antibiotic era. No definitive studies have been carried out till date to define the incidence of lung abscess from India and reliable epidemiological data are not available.
Differential Diagnosis
1. Non-infectious diseases
- Embolism with infarction
- Vasculitis
- Pulmonary neoplasm
- Pulmonary sequestration
- Bullae or cysts with air fluid level
2. Infections
- Infected bulla
- Infected pulmonary infarct
- Infected cyst
- Bronchiectasis
- Empyema with air fluid level
Prevention And Counselling
1. Measures for preventing aspiration of secretions in unconscious patients
2. Smoking cessation, good orodental hygiene
3. Early recognition of lung infections and institution of appropriate antibiotics in adequate dosage for appropriate duration.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
*Situation 1: At Secondary Hospital: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis
Symptoms
1. The clinical manifestations of lung abscess may become evident coincident with the initial presentation of pneumonia or other underlying condition, or may develop later in the course of the illness.
2. Conditions predisposing the patient for aspiration and development of lung abscess, such as altered sensorium, depressed cough and gag reflex, diseases of the oral cavity, gastrointestinal disease, and neurological disease are usually present.
3. Patients with primary lung abscess often have an ongoing episode of pneumonia of 2-3 weeks duration, or, a history of pneumonia in the recent past. Presenting symptoms include fever, cough, sputum, that may be putrid and foul smelling. Pleuritic chest pain, shoulder pain, heaviness in the chest is also usually evident. Patients may also complain of chills, night sweats, anorexia, haemoptysis, weight loss, and digital clubbing. In patients with a secondary lung abscess, the clinical manifestations can develop over 48 to 72 hours.
4. Patients with hepatopulmonary amoebiasis may manifest abdominal symptoms, such as, right hypochondrium pain, bowel symptoms, among others.
5. In patients with perforation of the liver abscess into the lung, cough and expectoration of odourless anchovy sauce sputum may be evident.
Signs
1. Patients with an acute lung abscess appear sick and toxic. New and focal respiratory signsmay be evident on physical examination of the chest. Presence of physical signs depends on the proximity lung abscess from the chest wall.
2. Signs due to complications, such as, pleural effusion, empyema, sepsis syndrome may also be present.
Investigations
1. Chest radiograph: A chest radiograph is essential to establish the diagnosis of lung abscess. Lung abscess appears as an irregularly shaped cavity with an air-fluid level. The lesion may be solitary (primary lung infection), or sometimes, multiple (metastatic infection). Rapid pulmonary cavitation within a dense segmental consolidation; and a rapidly enlarging nodular lesion, with or without cavitation suggest anaerobic infection.
2. Ultrasonography of the chest: Peripherally located lung abscesses, especially those in contact with pleura are detectable on ultrasonography of the chest.
Treatment:
not applicable
Standard Operating procedure
In Patient
1. General therapeutic measures
- Adequate drainage of the lung abscess is facilitated by encouraging the patient to cough and by chest physiotherapy and postural drainage.
- Antibiotic treatment: clindamycin administered intravenously in a dosage of 600 mg, eight hourly, followed by 150 to 300 mg orally four times daily is considered to be the preferred treatment of choice for lung abscess. Other antibiotic options include intravenous penicillin plus metronidazole and amoxycillin-clavulanate plus metronidazole.
- Antibiotic treatment is administered till the pulmonary infiltrates have resolved or until the residual lesion becomes small and stable; the duration of antibiotic treatment is usually for 6 to 8 weeks.
2. Supplemental oxygen therapy
In patients with hypoxaemia, spontaneous ventilation using a face mask with a high flow gas delivery system can be used to deliver a FIO2 of up to 0.5 to 0.6.
Out Patient
Not applicable
Referral criteria:
1. Patients not responding to antibiotic treatment.
2. Occurrence of complications of lung abscess, such as, metastatic brain abscess, sepsis, empyema, broncho-pleural fistula, pleura-cutaneous fistula, massive life-threatening haemoptysis, spontaneous rupture of the abscess into uninvolved lung segments, and failure to resolve.
Situation 2: At Tertiary hospital where higher-end technology is available
Clinical Diagnosis
Symptoms
1. The clinical manifestations of lung abscess may become evident coincident with the initial presentation of pneumonia or other underlying condition, or may develop later in the course of the illness.
2. Conditions predisposing the patient for aspiration and development of lung abscess, such as altered sensorium, depressed cough and gag reflex, diseases of the oral cavity, gastrointestinal disease, and neurological disease are usually present.
3. Patients with primary lung abscess often have an ongoing episode of pneumonia of 2-3 weeks duration, or, a history of pneumonia in the recent past. Presenting symptoms include fever, cough, sputum, that may be putrid and foul smelling. Pleuritic chest pain, shoulder pain, heaviness in the chest is also usually evident. Patients may also complain of chills, night sweats, anorexia, haemoptysis, weight loss, and digital clubbing. In patients with a secondary lung abscess, the clinical manifestations can develop over 48 to 72 hours.
4. Patients with hepatopulmonary amoebiasis may manifest abdominal symptoms, such as, right hypochondrium pain, bowel symptoms, among others.
5. In patients with perforation of the liver abscess into the lung, cough and expectoration of odourless anchovy sauce sputum may be evident.
Signs
1. Patients with an acute lung abscess appear sick and toxic. New and focal respiratory signsmay be evident on physical examination of the chest. Presence of physical signs depends on the proximity lung abscess from the chest wall.
2. Signs due to complications, such as, pleural effusion, empyema, sepsis syndrome may also be present.
Investigations
1. Chest radiograph : A chest radiograph is essential to establish the diagnosis of lung abscess. Lung abscess appears as an irregularly shaped cavity with an air-fluid level. The lesion may be solitary (primary lung infection), or sometimes, multiple (metastatic infection). Rapid pulmonary cavitation within a dense segmental consolidation; and a rapidly enlarging nodular lesion, with or without cavitation suggest anaerobic infection.
2. Ultrasonography of the chest : Peripherally located lung abscesses, especially those in contact with pleura are detectable on ultrasonography of the chest.
3. Computed tomography : computed tomography (CT) of the chest helps in delineating the size and location of abscesses. It also facilitates identifying associated empyema, and detecting other conditions such as pulmonary infarction, infected bulla, and raising the suspicion of a cavitating lung malignancy. In lung abscesses that fail to communicate with a bronchus, the characteristic air-fluid level within a cavity will not be seen and instead, a focal, ground-glass infiltrate with indistinct borders may be evident.
4. Establishing microbiological diagnosis :
- Ascertaining the microbiology of anaerobic infection of the lower airways requires a specimen devoid of contamination by the flora of the upper airways or quantitative cultures that can distinguish pathogenic bacteria from the normal flora.
- Specimens obtained from blind, deep suctioning via an endotracheal tube; radiologically guided, percutaenous transthoracic aspirates, specimens obtained at thoracotomy, quantitative cultures of specimens obtained at fiberoptic bronchoscopy (FOB), either by bronchoalveolar lavage (BAL) or with the protected double-lumen catheter with a protected sampling brush are subjected to microbiological examination. 3.If the abscess is associated with an empyema, then culture of the empyema fluid may help in isolating the aetiological organisms.
Treatment:
not applicable
Standard Operating procedure
In Patient
1. General therapeutic measures
- Adequate drainage of the lung abscess is facilitated by encouraging the patient to cough and by chest physiotherapy and postural drainage.
- Antibiotic treatment: clindamycin administered intravenously in a dosage of 600 mg, eight hourly, followed by 150 to 300 mg orally four times daily is considered to be the preferred treatment of choice for lung abscess. Other antibiotic options include intravenous penicillin plus metronidazole and amoxycillin-clavulanate plus metronidazole.
- Antibiotic treatment is administered till the pulmonary infiltrates have resolved or until the residual lesion becomes small and stable; the duration of antibiotic treatment is usually for 6 to 8 weeks.
2. Supplemental oxygen therapy
In patients with hypoxaemia, spontaneous ventilation using a face mask with a high flow gas delivery system can be used to deliver a FIO2 of up to 0.5 to 0.6.
3. Drainage procedures
Drainage procedures are usually reserved for patients with lung abscess who fail to respond to antibiotic therapy
- Percutaneous catheter drainage (for peripherally located lung abscess)
- Video-assisted thoracoscopic surgery (VATS)
4. Surgery
- Surgery is indicated if airway obstruction (e.g., due to a tumour or a foreign body) limits drainage. The surgical procedures performed include lobectomy, wedge resection or pneumonectomy.
- When associated empyema is present, adequate drainage with tube thoracostomy is required; in patients with multiloculated empyemas, open pleural drainage is indicated.
Out Patient
Not applicable.
WHO DOES WHAT? and TIMELINES
Doctor:
Diagnosis and Management including counseling
Nurse:
Implementation of orders, monitoring of patients and counseling
Technician:
Investigations
Resources Required For One Patient
| Situation | Human Resources | Investigations | Drugs & Consumables | Equipment |
| 1. | 1. Physician 2.Nurse 3.Radiographer | 1.Chest X-ray 2.Ultrasonography of chest 3. sputum smear and culture 4. Blood culture and sensitivity | 1. Oral and i.v. antibiotics 2. Streptokinase | 1. X-ray machine 2. USG machine 3. Intercostal tubes 4. Negative suction machines |
| 2. | Above plus 1. Intensivist 2.Interventional Radiologist 3.Thoracic Surgeon 4.Nurse and Technician for assisting with bronchsocopy 5.Nurse and Technician for assisting with interventional radiology procedures 6.Nursing staff trained in assisting thoracic surgery 7.Respiratory therapist | Above plus 1.CT chest 2.Interventional radiology procedures 3.Bronchoscopy 4.Conventional and molecular microbiological diagnostic methods 5.Fiberoptic bronchoscopy | Above plus 1.Catheters and tubes for drainage procedures 2.Disposables for use during interventional procedures/ VATS/ surgical intervention | Above plus 1. CT machine 2.Facilities for conducting interventional radiology procedures 3.Bronchoscope and facilities for performing interventional pulmonology procedures 4.Microbiology laboratory service with facilities for conventional and molecular diagnostic testing 5.Video-assisted thoracoscope 6.Thoracic surgery operating theatre; recovery room and ICU |
Guidelines by The Ministry of Health and Family Welfare :
Dr S.K. SHARMA AIIMS

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd