- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Lower Gastrointestinal Bleed - Standard Treatment Guidelines
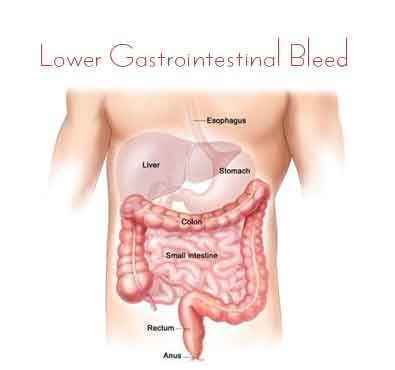
Lower GI bleeding is a common GI problem. It may present as acute lower GI bleed or may present as occult GI bleed leading to chronic GI blood loss. It may also present as a challenging problem in the form of obscure GI bleed.
The Ministry of Health and Family Welfare has issued the Standard Treatment Guidelines Gastroenterological Diseases for Lower Gastrointestinal Bleed. Following are the major recommendations :
Case definition:
Any bleeding beyond ligament of Treitz is called as lower GI bleed. Mid GI bleed is any bleed between ampulla of Vater and ileocaecal valve. The source of bleed is colonic in 80-90% of the cases and small intestinal in 1-10% of the cases
Incidence of The Condition In Our Country
It is less common than Upper GI bleed. Men are affected more commonly than women. An increased incidence is seen with increase in age. The incidence in Western countries is 20-30/10,000. Incidence data are not available for India
Differential Diagnosis
LGI bleed may present with a constellation of clinical symptoms like anaemia, haematochezia, maelena, maroon coloured blood in the stools with or without constitutional features. The common causes of LGI bleed in the Indian context include anorectal causes (haemorrhoids, anal fissures), acute self limiting colitis ( Shigella, E. coli), amoebiasis , enteric fever, colonic tuberculosis , inflammatory bowel disease ( ulcerative colitis and Crohn’s disease), solitary rectal ulcer syndrome , colon cancer, polyposis coli, radiation colitis, diverticular disease, NSAID induced bleed, Meckel’s diverticulum and ischaemic colitis .
Prevention And Counseling
Acute self limiting colitis and parasitic diseases are often food or water borne diseases and maintaining high levels of hygiene may prevent these diseases.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis:
History should include following points, which may aid in clinical diagnosis:
a) Age: Elderly are more predisposed to cancer colon, diverticular disease and ischaemic colitis. Pediatric age group is predisposed to bleed from rectal polyp or Meckel’s diverticulum.
b) History of fever : suggests infectious disease as a cause
c) H/o of altered bowel habits for a long duration suggests inflammatory bowel disease or intestinal tuberculosis
d) H/o constipation with bleed suggests haemorrhoidal bleed or solitary rectal ulcer syndrome
e) Constitutional symptoms – anorexia, pain abdomen, weight loss
f) History suggestive of partial intestinal or colonic obstruction
g) H/o of drugs – NSAIDS, anticoagulants
h) H/o of radiation, mainly to pelvic region in past
i) Past H/o of similar or less threatening LGI Bleed
j) Past H/o of endoscopic intervention e.g. polypectomy
Assess for
a) Type of blood per rectum - red, maroon or malaenic which depends upon source and rapidity of blood loss
b) Whether blood is mixed with stools, separate from stool or only blood is seen. Blood if separate from the stools suggests haemorrhoidal bleed or solitary rectal ulcer syndrome.
Investigations:
- Assess for signs of blood volume loss-Pulse rate, BP
- Assess for aetiology of bleed
a) Skin telengiectesia, Lymph nodes, abdominal tenderness, abdominal lump
b) Digital rectal examination to look for anorectal causes and stool colour
c) Proctoscopy to rule out haemorrhoids and evaluate rectal mucosa
- Assessment of other organ systems mainly cardiovascular and pulmonary
Treatment:
Standard Operating procedure
- Resuscitation and assessment go hand in hand
- Two large bore i.v.cannula or a central venous line if acute LGI bleed
- Start crystalloids and plasma expanders, arrange packed RBC
- Send samples for CBC, electrolytes, urea, coagulation profile and sample for grouping and cross match
- Ryle’s tube (RT) placement and check for RT aspirate
a. InPatient: Patients should be admitted if presenting with LGI bleed
b. OutPatient: If a patient presents with occult GI bleed and anaemia the management may be outpatient based if the anaemia is not very severe
c. DayCare: In occult GI bleed, the patient may be given blood transfusions to treat for symptoms resulting from anaemia and thereafter referred to a tertiary centre for further investigations
Referral criteria:
- Continuous active bleed
- Hemodynamic compromise either hypotension or orthostatic hypotension
- Transfusion requirement of >2 packed RBCs to maintain haemodynamic stability
- Presence with comorbid illness who require monitoring
- Obscure GI bleed where the cause of bleed needs to be ascertained
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis:
History should include following points, which may aid in clinical diagnosis:
a) Age: Elderly are more predisposed to cancer colon, diverticular disease and ischaemic colitis. Pediatric age group is predisposed to bleed from rectal polyp or Meckel’s diverticulum.
b) History of fever : suggests infectious disease as a cause
c) H/o of altered bowel habits for a long duration suggests inflammatory bowel disease or intestinal tuberculosis
d) H/o constipation with bleed suggests haemorrhoidal bleed or solitary rectal ulcer syndrome
e) Constitutional symptoms – anorexia, pain abdomen, weight loss
f) History suggestive of partial intestinal or colonic obstruction
g) H/o of drugs – NSAIDS, anticoagulants
h) H/o of radiation, mainly to pelvic region in past
i) Past H/o of similar or less threatening LGI Bleed
j) Past H/o of endoscopic intervention e.g. polypectomy
Assess for
a) Type of blood per rectum - red, maroon or malaenic which depends upon source and rapidity of blood loss
b) Whether blood is mixed with stools, separate from stool or only blood is seen. Blood if separate from the stools suggests haemorrhoidal bleed or solitary rectal ulcer syndrome.
Investigations:
Active LGI bleed:
UGI endoscopy
Colonoscopy
Angiography
Radio nuclide scan
Exploratory Laparotomy with intra-operative endoscopy
Occult/Obscure GI bleed:
Stool for occult blood
Stool for parasites
UGI endoscopy
Colonoscopy
Capsule endoscopy/Double balloon enteroscopy
Computed tomography (Enteroclysis)
Radionuclide scan Exploratory laparotomy with intra-operative endoscopy
Treatment:
Endoscopic therapy :10% to 15% of patients undergoing urgent colonoscopy receive endoscopic therapy
1. Injection therapy (epinephrine or saline)
2. Heater probe therapy
3. Argon plasma coagulation
4. Haemoclips
Radiology techniques
1. Vasopressin infusion
2. Selective embolisation: Definitive means of controlling hemorrhage
– stops bleeding 67-100%
– Re-bleed 15%-40%
– High incidence of bowel ischemia
3. Super selective embolisation Target artery - the vasa recta; also within the marginal arteries and the distal intestinal arcades A number of primary embolic agents
a. Microcoils
b. Gelatin sponge particles
c. Poly vinyl sponge particles
Surgery
1. Bleeding refractory to other therapies
2. Requirement of more than 8 units of blood over 24 hours
3. Hemodynamic instability
4. Re-bleeding after non-operative treatment, esp if localized
5. Segmentectomy if site of bleed is known
6. Right hemicolectomy if bleed from unknown
Referral centre:
Outcomes at a tertiary referral centre 49 Mortality at 3 yr follow up 19%
- Most patients stop bleeding spontaneously
- Rebleed occurs in 10% to 40% of patients
- Between 5% and 50% of patients with persistent bleeding require surgical hemostasi
Guidelines by The Ministry of Health and Family Welfare :
Dr Vineet Ahuja Deptt of Gastroenterology, All India Institute of Medical Sciences, New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd