- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Low platelet count does not increase bleeding risk in PCI
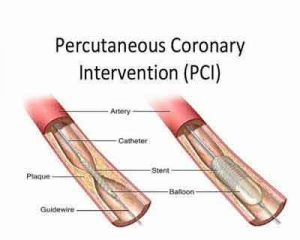
China: Thrombocytopenia (low platelet levels in the blood) is a common occurrence among patients undergoing elective percutaneous coronary intervention (PCI). However, a new study published in the journal Catheterization and Cardiovascular Interventions has found that thrombocytopenia (TP) is not liked to long-term risks, particularly bleeding risk from PCI.
- A low platelet count of less than 150 × 109/L was common, seen in about one in eight (12.76%) of the 9,897 consecutive PCI patients.
- Similar adverse event rates over 30 months were observed whether patients had normal or low platelet counts at baseline:
- Death: 1.2% vs 1.0%
- Cardiac death: 0.6% vs 0.6%
- MI: 1.1% vs 0.7%
- Target vessel revascularization: 5.3% vs 4.6%
- Bleeding: 6.7% vs 6.6%
- Ischemic stroke: 1.5% vs 1.7%
- Major adverse cardiovascular events: 6.8% vs 5.9%
- Thrombocytopenia was independently associated with advanced age, male sex, prior PCI, prior myocardial infarction, and diabetes.
"Although baseline thrombocytopenia was common among patients who underwent elective PCI, it did not appear to have a clinically significant effect on long-term adverse outcomes, [in] particular bleeding risk," write the authors, noting that not one of the 91 patients with moderate or severe thrombocytopenia experienced major bleeding.
These good outcomes for PCI patients with thrombocytopenia contrasted with the strong association with ischemic events in the ACUITY and HORIZONS-AMI trials noted the investigators. This may be because the Chinese study was unique in two ways: study population and duration of antiplatelet therapy.
Nearly all patients in the study got aspirin and clopidogrel (Plavix). Given the findings, 12 months of dual antiplatelet therapy (DAPT) may be safe for patients with thrombocytopenia who have no hematologic diseases or history of GI bleeding, the authors said.
In general, operators can balance thrombotic and bleeding risks during PCI by using a radial approach with second-generation drug-eluting stents, as well as opting for proton pump inhibitors while avoiding glycoprotein IIb-IIIa inhibitors, they suggested. Among the P2Y12 inhibitors, clopidogrel (Plavix) would be the "agent of choice" in patients with thrombocytopenia getting DAPT, they added.
Dou and colleagues acknowledged that the limitations to their post hoc analysis included having relatively few patients with moderate or severe thrombocytopenia and not systematically recording the cause of platelet dysfunction.
"Our results indicated that it seems to be feasible for patients with mild to moderate thrombocytopenia to receive elective PCI as well as the guideline‐recommended duration of anti‐platelet therapy," concluded the authors.
For further reference log on to https://doi.org/10.1002/ccd.28030

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd