- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Long term Stroke rate lower after PCI vs CABG in CAD : JACC
The rates of stroke are lower after five years in patients with multivessel or left main coronary artery disease who underwent percutaneous coronary intervention (PCI) as compared to those subjected to coronary artery bypass grafting (CABG).The results also revealed that strokes occurring within 30 days after the procedures were strongly associated with increased long-term mortality, with a rate approaching 50% at 5 years.
These are the results of a study published in the Journal of the American College of Cardiology (JACC).
Stuart J. Head, Erasmus Medical Center in Rotterdam, Netherlands, and colleagues conducted the study to compare stroke rates after CABG and PCI and the impact of procedural stroke on long-term mortality.
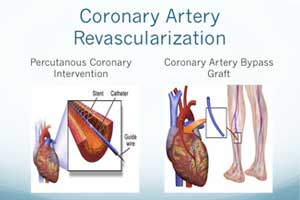
CABG and PCI are used for coronary revascularization in patients with multivessel and left main coronary artery disease. One of the most feared complications of revascularization is a stroke.
Stroke is among the most feared complications of revascularization. Due to its infrequency, studies employing a large number of patients are required to spot differences in rates of stroke between PCI and CABG.
Read Also: Complete revascularization PCI has better outcomes than culprit-only PCI
For the study, the investigators performed a collaborative individual patient-data pooled analysis of 11 randomized clinical trials that compared PCI with CABG using stents. The 30-day and 5-year stroke rates were compared between CABG and PCI using a random-effects Cox proportional hazards model, stratified by trial. The impact of stroke on 5-year mortality was explored.
The analysis included 11,518 patients randomly assigned to PCI (n = 5,753) or CABG (n = 5,765) with a mean follow-up of 3.8 ± 1.4 years during which a total of 293 strokes occurred.
Key Findings:
- At 30 days, the rate of stroke was 0.4% after PCI and 1.1% after CABG (hazard ratio [HR]: 0.33; 95% confidence interval [CI]: 0.20 to 0.53).
- At 5-year follow-up, stroke remained significantly lower after PCI than after CABG (2.6% vs. 3.2%; HR: 0.77; 95% CI: 0.61 to 0.97).
- Rates of stroke between 31 days and 5 years were comparable: 2.2% after PCI versus 2.1% after CABG (HR: 1.05; 95% CI: 0.80 to 1.38).
- No significant interactions between treatment and baseline clinical or angiographic variables for the 5-year rate of stroke were present, except for diabetic patients (PCI: 2.6% vs. CABG: 4.9%) and nondiabetic patients (PCI: 2.6% vs. CABG: 2.4%).
- Patients who experienced a stroke within 30 days of the procedure had significantly higher 5-year mortality versus those without a stroke, both after PCI (45.7% vs. 11.1%, p < 0.001) and CABG (41.5% vs. 8.9%).
"Our results demonstrate that 5-year stroke rates are significantly lower after PCI compared with CABG, driven by a reduced risk of stroke in the 30-day post-procedural period but a similar risk of stroke between 31 days and 5 years. The greater risk of stroke after CABG compared with PCI was confined to patients with multivessel disease and diabetes. Five-year mortality was markedly higher for patients experiencing a stroke within 30 days after revascularization," concluded the authors.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd