- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Latest guidelines on management of Idiopathic intracranial hypertension
A team of researchers including Susan P. Mollan, Metabolic Neurology, Institute of Metabolism and Systems Research, University of Birmingham, Birmingham, UK, and colleagues have developed consensus guidelines for optimal management of idiopathic intracranial hypertension (IIH).
The guidelines are published in the Journal of Neurology, Neurosurgery, and Psychiatry.
KEY RECOMMENDATIONS:
Diagnostic Principles
For optimal investigation of patients with papilloedema, there must be clear communication between clinicians for seamless joint investigation between the various specialties. The aims of investigations of papilloedema are to:
- Find any underlying treatable cause in a timely manner
- Protect the vision and ensure timely re-examination when vision is at risk
- Enable onward care of the patient with the input from the most appropriate experienced clinician.
Investigation of papilloedema
- Blood pressure must be measured to exclude malignant hypertension, as defined as a diastolic blood pressure greater than or equal to 120 mm Hg or systolic blood pressure greater than or equal to 180 mm Hg.
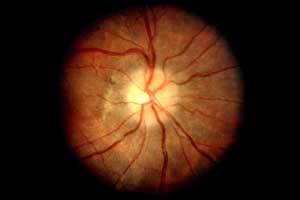
- Ophthalmology examination: all patients should have papilloedema confirmed and an assessment made of the imminent risk to their visual function. The following should be recorded in the presence of papilloedema:
- visual acuity
- pupil examination
- intraocular pressure (to exclude hypotony, a rare cause for disc swelling)
- formal visual field test (perimetry)
- dilated fundal examination to grade the severity of the papilloedema and exclude ocular causes for disc swelling.
- An experienced clinician should be consulted early before invasive tests are performed.
- Neurological examination
- Record cranial nerve examination. Where IIH is suspected, typically there should be no cranial nerve involvement other than sixth cranial nerve palsy/palsies.
- Should other cranial nerves and/or other pathological findings be involved, an alternative diagnosis should be considered.
- Neuroimaging
- Urgent MRI brain within 24 hours; if unavailable within 24 hours, then urgent CT brain with subsequent MRI brain if no lesion identified.
- There should be no evidence of hydrocephalus, mass, structural, vascular lesion and no abnormal meningeal enhancement.
- CT or MR venography is mandatory to exclude cerebral sinus thrombosis within 24 hours.
- Characteristics of raised intracranial pressure may be seen on neuroimaging; these are not pathognomonic of IIH.
- Where there is diagnostic uncertainty regarding interpretation of the venogram findings, an experienced radiologist should be consulted.
- Lumbar puncture
- Following normal imaging, all patients with papilloedema should have a lumbar puncture to check opening pressure and ensure contents are normal.
- The lumboperitoneal (LP) opening pressure should be measured in the lateral decubitus position. Following needle insertion into the CSF space, the pressure recording should occur with the patient relaxed and the legs extended. The CSF level should be allowed to settle before taking the reading.
- The CSF analysis should be tailored to the presentation but should at a minimum include CSF protein, glucose, and cell count.
- A clear explanation of the LP should be given to patients to reduce fear and anxiety about the procedure.
- Where difficulty exists in performing the LP, the length of the procedure should be balanced by the comfort of the individual patient.
- Should the LP not be successful, a guided LP could then be considered (ultrasound or X-ray).
- The diagnostic criteria mandate a cut-off opening pressure of >25 cm CSF for diagnosing IIH.
- The LP opening pressure should not be interpreted in isolation when diagnosing IIH.
Management Principles
For optimal management of patients with IIH, there must be clear communication between clinicians for seamless joint care between the various specialties. Weight loss reduces ICP and has been shown to be effective in improving papilloedema and headaches. The main principles of management of IIH are:
- to treat the underlying disease
- to protect the vision
- to minimize the headache morbidity
Treat the Underlying Disease
- Once definite IIH is diagnosed, all patients with a BMI >30 kg/m2 should be counseled about weight management at the earliest opportunity. This should be done with sensitivity.
- The amount of weight loss required to put the disease into remission is not known. It is noted that in the year preceding a diagnosis of IIH is associated with 5%–15% weight gain and up to 15% of weight loss was required to put IIH into remission in one cohory.
- Patients should be referred to a community weight management programme or a hospital-based weight programme.
Protect the Vision
- Where there is evidence of declining visual function, the acute management to preserve vision is surgical.
- A temporizing measure of a lumbar drain could be useful to protect the vision while planning urgent surgical treatment.
- There is evidence that many of the surgical procedures, such as CSF diversion and optic nerve sheath fenestration (ONSF), work well in the short term. While they are working, the underlying disease should be modified with weight loss.
- The role of neurovascular stenting in IIH is not yet established.
- Long-term antithrombotic therapy is required for longer than 6 months following neurovascular stenting treatment.
- Serial lumbar punctures are not recommended for the management of IIH.
- The IIH Treatment Trial reported the use of acetazolamide with a low-sodium weight-reduction diet compared with diet alone resulted in modest improvement in visual field function in patients with a mild visual loss. The IIHTT also reported improved quality of life outcomes at 6 months with acetazolamide.
Minimize the Headache Morbidity
- Patients must be informed, at the earliest opportunity, of the potential issues of painkiller overuse that can lead to medication overuse headache.
- Short-term painkillers may be helpful in the first few weeks following diagnosis.
- Opioids should not be prescribed for headaches.
- Greater occipital nerve blocks may be considered helpful by some, but there is a lack of evidence and consensus.
- Acetazolamide has not been shown to be effective for the treatment of headache alone.
- Lumbar punctures are not typically recommended for treatment of headache in IIH.
Clinical Care
Chronic Problems that Need to be Addressed in IIH
- All of these patients require recognition that they have been diagnosed with a rare disease and need appropriate support to deal with the psychological burden of living with a chronic condition.
- The patient with IIH may have significantly higher levels of anxiety and depression and a lower quality of life. This may be as a response to chronic pain. This needs recognition and appropriate management.
- Sleep apnoea is frequently reported in this group, and referral to respiratory service may be appropriate.
Managing IIH in Pregnancy
Drug Treatments in the Pregnant Patients with IIH
- A clear risk−benefit assessment regarding the necessity of acetazolamide treatment during pregnancy should be discussed with the patient as perinatal exposure in rodents has reported teratogenic effects.
- With the limited evidence, it is difficult to make any safe recommendations on using acetazolamide during pregnancy and its manufacturers do not recommend its use.
- Topiramate should not be used in pregnancy. There is clear evidence of a higher rate of fetal abnormalities following its use.
- If a patient on topiramate becomes pregnant, they should reduce and discontinue it as soon as possible in line with manufacturers recommendations.
For further information follow the link: 10.1136/jnnp-2017-317440

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd