- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
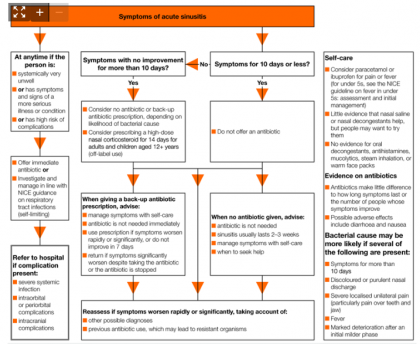
Latest acute sinusitis guideline : antimicrobial prescribing by NICE
Symptoms and signs
Common symptoms and signs
- Adults with acute sinusitis usually present with:
- nasal blockage or congestion
- nasal discharge
- dental or facial pain or pressure
- reduction or loss of the sense of smell
- Children (particularly young children) often present with non‑specific symptoms in the upper respiratory tract. Symptoms of acute sinusitis in children may include the following, but these can be present for many upper respiratory tract infections:
- nasal blockage or congestion
- discoloured nasal discharge
- cough during the day or at night
Factors that might make a bacterial cause more likely
- It is difficult to distinguish viral and bacterial acute sinusitis. A bacterial cause may be more likely if several of the following are present:
- symptoms for more than 10 days
- discoloured or purulent nasal discharge
- severe localised unilateral pain (particularly pain over teeth and jaw)
- fever
- marked deterioration after an initial milder phase
Managing acute sinusitis
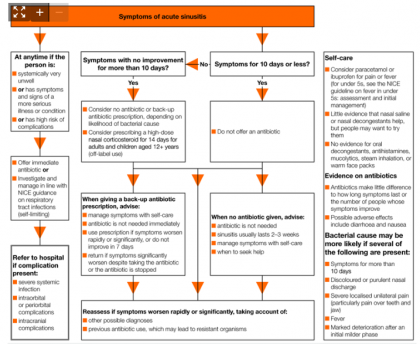 Image Source: NICE
Image Source: NICEPeople presenting with symptoms for around 10 days or less
- Do not offer an antibiotic prescription
- Give advice about:
- the usual course of acute sinusitis (2 to 3 weeks)
- an antibiotic not being needed
- managing symptoms, including fever, with self-care (see the recommendations on self-care)
- seeking medical help if symptoms worsen rapidly or significantly, do not improve after 3 weeks, or they become systemically very unwell
- Reassess if symptoms worsen rapidly or significantly, taking account of:
- alternative diagnoses such as a dental infection
- any symptoms or signs suggesting a more serious illness or condition
People presenting with symptoms for around 10 days or more with no improvement
- Consider prescribing a high-dose nasal corticosteroid* for 14 days for adults and children aged 12 years and over, being aware that nasal corticosteroids:
- may improve symptoms but are not likely to affect how long they last
- could cause systemic effects, particularly in people already taking another corticosteroid
- may be difficult for people to use correctly
- Consider no antibiotic prescription or a back-up antibiotic prescription (see the recommendations on choice of antibiotic), taking account of:
- evidence that antibiotics make little difference to how long symptoms last, or the proportion of people with improved symptoms
- withholding antibiotics is unlikely to lead to complications
- possible adverse effects, particularly diarrhoea and nausea
- factors that might make a bacterial cause more likely (see symptoms and signs)
- When a back-up antibiotic prescription is given, give verbal and written advice about:
- managing symptoms, including fever, with self-care (see the recommendations on self-care)
- an antibiotic not being needed immediately
- using the back-up prescription if symptoms do not improve within 7 days or if they worsen rapidly or significantly at any time
- seeking medical help if symptoms worsen rapidly or significantly despite taking the antibiotic, or the antibiotic has been stopped because it was not tolerated
- Reassess if symptoms worsen rapidly or significantly despite taking treatment, taking account of:
- alternative diagnoses such as a dental infection
- any signs or symptoms suggesting a more serious illness or condition
- previous antibiotic use, which may lead to resistant organisms
People presenting at any time who are systemically very unwell, have symptoms and signs of a more serious illness or condition or are at high risk of complications
- Offer an immediate antibiotic prescription (see the recommendations on choice of antibiotic) or further appropriate investigation and management in line with the NICE guideline on respiratory tract infections (self-limiting): prescribing antibiotics
- Refer people to hospital if they have symptoms and signs of acute sinusitis associated with any of the following:
- a severe systemic infection (see the NICE guideline on sepsis)
- intraorbital or periorbital complications, including periorbital oedema or cellulitis, a displaced eyeball, double vision, ophthalmoplegia, or newly reduced visual acuity
- intracranial complications, including swelling over the frontal bone, symptoms or signs of meningitis, severe frontal headache, or focal neurological signs.
Choice of antibiotic
- When prescribing antibiotics for acute sinusitis:
- follow the recommendations in table 1 for adults aged 18 years and over
- follow the recommendations in table 2 for children and young people under 18 years.
| Antibiotic† | Dosage and course length for adults |
|---|---|
| First choice | |
| Phenoxymethylpenicillin | 500 mg four times a day for 5 days |
| First choice if systemically very unwell, symptoms and signs of a more serious illness or condition, or at high risk of complications | |
| Co-amoxiclav | 500/125 mg three times a day for 5 days |
| Alternative first choices for penicillin allergy or intolerance | |
| Doxycycline | 200 mg on first day, then 100 mg once a day for 4 days (5-day course in total) |
| Clarithromycin | 500 mg twice a day for 5 days |
| Erythromycin (in pregnancy) | 250 mg to 500 mg four times a day or 500 mg to 1000 mg twice a day for 5 days |
| Second choice (worsening symptoms on first choice taken for at least 2 to 3 days) | |
| Co-amoxiclav‡ | 500/125 mg three times a day for 5 days |
| Alternative second choice for penicillin allergy or intolerance, or worsening symptoms on second choice taken for at least 2 to 3 days | |
| Consult local microbiologist | |
| † See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment, renal impairment, pregnancy and breast-feeding. ‡ If co-amoxiclav has been used as first choice, consult local microbiologist for advice on second choice. | |
| Antibiotic§ | Dosage and course length for children and young people| |
|---|---|
| First choice | |
| Phenoxymethylpenicillin | 1 to 11 months, 62.5 mg four times a day for 5 days 1 to 5 years, 125 mg four times a day for 5 days 6 to 11 years, 250 mg four times a day for 5 days 12 to 17 years, 500 mg four times a day for 5 days |
| First choice if systemically very unwell, symptoms and signs of a more serious illness or condition, or at high risk of complications | |
| Co-amoxiclav | 1 to 11 months, 0.25 ml/kg of 125/31 suspension three times a day for 5 days 1 to 5 years, 5 ml of 125/31 suspension three times a day or 0.25 ml/kg of 125/31 suspension three times a day for 5 days 6 to 11 years, 5 ml of 250/62 suspension three times a day or 0.15 ml/kg of 250/62 suspension three times a day for 5 days 12 to 17 years, 250/125 mg three times a day or 500/125 mg three times a day for 5 days |
| Alternative first choice for penicillin allergy or intolerance | |
| Clarithromycin | Under 8 kg, 7.5 mg/kg twice a day for 5 days 8 to 11 kg, 62.5 mg twice a day for 5 days 12 to 19 kg, 125 mg twice a day for 5 days 20 to 29 kg, 187.5 mg twice a day for 5 days 30 to 40 kg, 250 mg twice a day for 5 days 12 to 17 years, 250 mg twice a day or 500 mg twice a day for 5 days |
| Doxycycline¶ | 12 to 17 years, 200 mg on first day, then 100 mg once a day for 4 days (5-day course in total) |
| Second choice (worsening symptoms on first choice taken for at least 2 to 3 days) | |
| Co-amoxiclav** | As above |
| Alternative second choice for penicillin allergy or intolerance, or worsening symptoms on second choice taken for at least 2 to 3 days | |
| Consult local microbiologist | |
| § See BNF for children for appropriate use and dosing in specific populations, for example, hepatic impairment and renal impairment. | The age bands apply to children of average size and, in practice, the prescriber will use the age bands in conjunction with other factors such as the severity of the condition being treated and the child’s size in relation to the average size of children of the same age. ¶ Doxycycline is contraindicated in children under 12 years. ** If co-amoxiclav used as first choice, consult local microbiologist for advice on second choice. | |
Self-care
- Consider paracetamol or ibuprofen for pain or fever (assess and manage children aged under 5 who present with fever as outlined in the NICE guideline on fever in under 5s)
- Explain that some people may wish to try nasal saline or nasal decongestants, although there is not enough evidence to show that they help to relieve nasal congestion
- Explain that no evidence was found for using oral decongestants, antihistamines, mucolytics, steam inhalation, or warm face packs
* High-dose nasal corticosteroids used in the studies were mometasone 200 micrograms twice a day and fluticasone 110 micrograms twice a day. Nasal corticosteroids are not licensed for treating acute sinusitis, so use for this indication would be off-label. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council’s Good practice in prescribing and managing medicines and devices for further information.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd