- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Intravenous fluid therapy in adults in hospital: NICE Guidelines
Many adult hospital inpatients need intravenous (IV) fluid therapy to prevent or correct problems with their fluid and/or electrolyte status. Deciding on the optimal amount and composition of IV fluids to be administered and the best rate at which to give them can be a difficult and complex task, and decisions must be based on careful assessment of the patient's individual needs.
National Institute for Health and Care Excellence, UK (NICE) has updated its guidelines on Intravenous fluid therapy in adults in hospital in May 2017. Following are the major recommendations
1.1 Principles and protocols for intravenous fluid therapy
The assessment and management of patients' fluid and electrolyte needs is fundamental to good patient care.
1.1.1 Assess and manage patients' fluid and electrolyte needs as part of every ward review. Provide intravenous (IV) fluid therapy only for patients whose needs cannot be met by oral or enteral routes, and stop as soon as possible.
1.1.2 Skilled and competent healthcare professionals should prescribe and administer IV fluids, and assess and monitor patients receiving IV fluids
1.1.3 When prescribing IV fluids, remember the 5 Rs: Resuscitation, Routine maintenance, Replacement, Redistribution and Reassessment.
1.1.4 Offer IV fluid therapy as part of a protocol (see Algorithms for IV fluid therapy):
- Assess patients' fluid and electrolyte needs following Algorithm 1: Assessment.
- If patients need IV fluids for fluid resuscitation, follow Algorithm 2: Fluid resuscitation.
- If patients need IV fluids for routine maintenance, follow Algorithm 3: Routine maintenance.
- If patients need IV fluids to address existing deficits or excesses, ongoing abnormal losses or abnormal fluid distribution, follow Algorithm 4: Replacement and redistribution.
Algorithms for IV fluid therapy
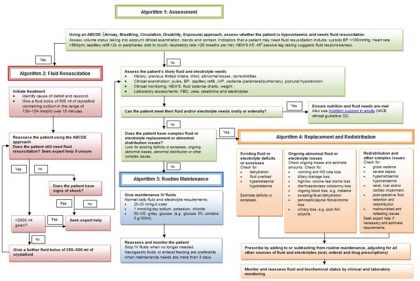 Image Source: NICE
Image Source: NICE1.1.5 Include the following information in IV fluid prescriptions:
- The type of fluid to be administered.
- The rate and volume of fluid to be administered.
1.1.6 Patients should have an IV fluid management plan, which should include details of:
- the fluid and electrolyte prescription over the next 24 hours
- the assessment and monitoring plan.Initially, the IV fluid management plan should be reviewed by an expert daily. IV fluid management plans for patients on longer-term IV fluid therapy whose condition is stable may be reviewed less frequently.
1.1.7 When prescribing IV fluids and electrolytes, take into account all other sources of fluid and electrolyte intake, including any oral or enteral intake, and intake from drugs, IV nutrition, blood and blood products.
1.1.8 Patients have a valuable contribution to make to their fluid balance. If a patient needs IV fluids, explain the decision, and discuss the signs and symptoms they need to look out for if their fluid balance needs adjusting. If possible or when asked, provide written information (for example, NICE's Information for the public), and involve the patient's family members or carers (as appropriate).
1.2 Assessment and monitoring
Initial assessment
1.2.1 Assess whether the patient is hypovolaemic. Indicators that a patient may need urgent fluid resuscitation include:
- systolic blood pressure is less than 100 mmHg
- heart rate is more than 90 beats per minute
- capillary refill time is more than 2 seconds or peripheries are cold to touch
- respiratory rate is more than 20 breaths per minute
- National Early Warning Score (NEWS) is 5 or more
- passive leg raising suggests fluid responsiveness.
1.2.2 Assess the patient's likely fluid and electrolyte needs from their history, clinical examination, current medications, clinical monitoring and laboratory investigations:
- History should include any previous limited intake, thirst, the quantity and composition of abnormal losses (see Diagram of ongoing losses), and any comorbidities, including patients who are malnourished and at risk of refeeding syndrome .
- Clinical examination should include an assessment of the patient's fluid status, including:
- pulse, blood pressure, capillary refill and jugular venous pressure
- presence of pulmonary or peripheral oedema
- presence of postural hypotension.
- Clinical monitoring should include current status and trends in:
- NEWS
- fluid balance charts
- weight.
- Laboratory investigations should include current status and trends in:
- full blood count
- urea, creatinine and electrolytes.
Reassessment
1.2.3 If patients are receiving IV fluids for resuscitation, reassess the patient using the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure), monitor their respiratory rate, pulse, blood pressure and perfusion continuously, and measure their venous lactate levels and/or arterial pH and base excess according to guidance on advanced life support .
1.2.4 All patients continuing to receive IV fluids need regular monitoring. This should initially include at least daily reassessments of clinical fluid status, laboratory values (urea, creatinine and electrolytes) and fluid balance charts, along with weight measurement twice weekly. Be aware that:
- Patients receiving IV fluid therapy to address replacement or redistribution problems may need more frequent monitoring.
- Additional monitoring of urinary sodium may be helpful in patients with high-volume gastrointestinal losses. (Reduced urinary sodium excretion [less than 30 mmol/l] may indicate total body sodium depletion even if plasma sodium levels are normal. Urinary sodium may also indicate the cause of hyponatraemia, and guide the achievement of a negative sodium balance in patients with oedema. However, urinary sodium values may be misleading in the presence of renal impairment or diuretic therapy.)
- Patients on longer-term IV fluid therapy whose condition is stable may be monitored less frequently, although decisions to reduce monitoring frequency should be detailed in their IV fluid management plan.
1.2.5 If patients have received IV fluids containing chloride concentrations greater than 120 mmol/l (for example, sodium chloride 0.9%), monitor their serum chloride concentration daily. If patients develop hyperchloraemia or acidaemia, reassess their IV fluid prescription and assess their acid–base status. Consider less frequent monitoring for patients who are stable.
1.2.6 Clear incidents of fluid mismanagement (for example, unnecessarily prolonged dehydration or inadvertent fluid overload due to IV fluid therapy) should be reported through standard critical incident reporting to encourage improved training and practice .
1.2.7 If patients are transferred to a different location, reassess their fluid status and IV fluid management plan on arrival in the new setting.
1.3 Resuscitation
1.3.1 If patients need IV fluid resuscitation, use crystalloids that contain sodium in the range 130–154 mmol/l, with a bolus of 500 ml over less than 15 minutes.
1.3.2 Do not use tetrastarch for fluid resuscitation.
1.3.3 Consider human albumin solution 4–5% for fluid resuscitation only in patients with severe sepsis.
1.4 Routine maintenance
1.4.1 If patients need IV fluids for routine maintenance alone, restrict the initial prescription to:
- 25–30 ml/kg/day of water and
- approximately 1 mmol/kg/day of potassium[3], sodium and chloride and
- approximately 50–100 g/day of glucose to limit starvation ketosis. For more information see IV fluid prescription for routine maintenance over a 24-hour period.
1.4.2 For patients who are obese, adjust the IV fluid prescription to their ideal body weight. Use lower range volumes per kg (patients rarely need more than a total of 3 litres of fluid per day) and seek expert help if their BMI is more than 40 kg/m2.
1.4.3 Consider prescribing less fluid (for example, 20–25 ml/kg/day fluid) for patients who:
- are older or frail
- have renal impairment or cardiac failure
- are malnourished and at risk of refeeding syndrome
1.4.4 When prescribing for routine maintenance alone, consider using 25–30 ml/kg/day sodium chloride 0.18% in 4% glucose with 27 mmol/l potassium on day 1 (there are other regimens to achieve this). Prescribing more than 2.5 litres per day increases the risk of hyponatraemia. These are initial prescriptions and further prescriptions should be guided by monitoring.
1.4.5 Consider delivering IV fluids for routine maintenance during daytime hours to promote sleep and wellbeing.
1.5 Replacement and redistribution
1.5.1 Adjust the IV prescription (add to or subtract from maintenance needs) to account for existing fluid and/or electrolyte deficits or excesses, ongoing losses (see Diagram of ongoing losses) or abnormal distribution.
1.5.2 Seek expert help if patients have a complex fluid and/or electrolyte redistribution issue or imbalance, or significant comorbidity, for example:
- gross oedema
- severe sepsis
- hyponatraemia or hypernatraemia
- renal, liver and/or cardiac impairment
- post-operative fluid retention and redistribution
- malnourished and refeeding issues
1.6 Training and education
1.6.1 Hospitals should establish systems to ensure that all healthcare professionals involved in prescribing and delivering IV fluid therapy are trained on the principles covered in this guideline, and are then formally assessed and reassessed at regular intervals to demonstrate competence in:
- understanding the physiology of fluid and electrolyte balance in patients with normal physiology and during illness
- assessing patients' fluid and electrolyte needs (the 5 Rs: Resuscitation, Routine maintenance, Replacement, Redistribution and Reassessment)
- assessing the risks, benefits and harms of IV fluids
- prescribing and administering IV fluids
- monitoring the patient response
- evaluating and documenting changes and
- taking appropriate action as required.
1.6.2 Healthcare professionals should receive training and education about, and be competent in, recognising, assessing and preventing consequences of mismanaged IV fluid therapy, including:
- pulmonary oedema
- peripheral oedema
- volume depletion and shock.
1.6.3 Hospitals should have an IV fluids lead, responsible for training, clinical governance, audit and review of IV fluid prescribing and patient outcomes.
Consequences of fluid mismanagement to be reported as critical incidents
| Consequence of fluid mismanagement | Identifying features | Time frame of identification |
| Hypovolaemia |
| Before and during IV fluid therapy |
| Pulmonary oedema (breathlessness during infusion) |
| During IV fluid therapy or within 6 hours of stopping IV fluids |
| Hyponatraemia |
| During IV fluid therapy or within 24 hours of stopping IV fluids |
| Hypernatraemia |
| During IV fluid therapy or within 24 hours of stopping IV fluids |
| Peripheral oedema |
| During IV fluid therapy or within 24 hours of stopping IV fluids |
| Hyperkalaemia |
| During IV fluid therapy or within 24 hours of stopping IV fluids |
| Hypokalaemia |
| During IV fluid therapy or within 24 hours of stopping IV fluids |
Source: This table was drafted based on the consensus decision of the members of the Guideline Development Group. Weight-based potassium prescriptions should be rounded to the nearest common fluids available (for example, a 67 kg person should have fluids containing 20 mmol and 40 mmol of potassium in a 24-hour period). Potassium should not be added to intravenous fluid bags as this is dangerous.
IV fluid prescription (by body weight) for routine maintenance over a 24‑hour period
| Body weight | Water | Sodium, chloride, potassium | Body weight | Water | Sodium, chloride, potassium | |
| kg | 25–30 ml/kg/day | approx. 1 mmol/kg/day of each | kg | 25–30ml/kg/day | approx. 1 mmol/kg/day of each | |
| 40 | 1000–1200 | 40 | 71 | 1775–2130 | 71 | |
| 41 | 1025–1230 | 41 | 72 | 1800–2160 | 72 | |
| 42 | 1050–1260 | 42 | 73 | 1825–2190 | 73 | |
| 43 | 1075–1290 | 43 | 74 | 1850–2220 | 74 | |
| 44 | 1100–1320 | 44 | 75 | 1875–2250 | 75 | |
| 45 | 1125–1350 | 45 | 76 | 1900–2280 | 76 | |
| 46 | 1150–1380 | 46 | 77 | 1925–2310 | 77 | |
| 47 | 1175–1410 | 47 | 78 | 1950–2340 | 78 | |
| 48 | 1200–1440 | 48 | 79 | 1975–2370 | 79 | |
| 49 | 1225–1470 | 49 | 80 | 2000–2400 | 80 | |
| 50 | 1250–1500 | 50 | 81 | 2025–2430 | 81 | |
| 51 | 1275–1530 | 51 | 82 | 2050–2460 | 82 | |
| 52 | 1300–1560 | 52 | 83 | 2075–2490 | 83 | |
| 53 | 1325–1590 | 53 | 84 | 2100–2520 | 84 | |
| 54 | 1350–1620 | 54 | 85 | 2125–2550 | 85 | |
| 55 | 1375–1650 | 55 | 86 | 2150–2580 | 86 | |
| 56 | 1400–1680 | 56 | 87 | 2175–2610 | 87 | |
| 57 | 1425–1710 | 57 | 88 | 2200–2640 | 88 | |
| 58 | 1450–1740 | 58 | 89 | 2225–2670 | 89 | |
| 59 | 1475–1770 | 59 | 90 | 2250–2700 | 90 | |
| 60 | 1500–1800 | 60 | 91 | 2275–2730 | 91 | |
| 61 | 1525–1830 | 61 | 92 | 2300–2760 | 92 | |
| 62 | 1550–1860 | 62 | 93 | 2325–2790 | 93 | |
| 63 | 1575–1890 | 63 | 94 | 2350–2820 | 94 | |
| 64 | 1600–1920 | 64 | 95 | 2375–2850 | 95 | |
| 65 | 1625–1950 | 65 | 96 | 2400–2880 | 96 | |
| 66 | 1650–1980 | 66 | 97 | 2425–2910 | 97 | |
| 67 | 1675–2010 | 67 | 98 | 2450–2940 | 98 | |
| 68 | 1700–2040 | 68 | 99 | 2475–2970 | 99 | |
| 69 | 1725–2070 | 69 | 100 | 2500–3000 | 100 | |
| 70 | 1750–2100 | 70 | >100 | 2500–3000 | 100 | |
| Add 50–100 grams/day glucose (e.g. glucose 5% contains 5g/100ml). For special considerations refer to the recommendations for routine maintenance. Weight-based potassium prescriptions should be rounded to the nearest common fluids available (for example, a 67 kg person should have fluids containing 20 mmol and 40 mmol of potassium in a 24-hour period). Potassium should not be added to intravenous fluid bags as this is dangerous. | ||||||
Source: NICE
To Read full guidelines click on the link given below.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd