- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Inguinal hernia treatment in children: Standard Treatment Guidelines
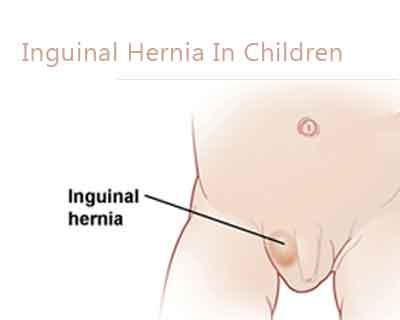
Inguinal hernia is suspected in any child with a swelling in the inguinoscrotal region. Inguinal hernia repair is one of the most common pediatric operations performed. Most hernias that present at birth or in childhood are indirect inguinal hernias. All pediatric inguinal hernias require operative treatment to prevent the development of complications, such as inguinal hernia incarceration or strangulation. The Ministry of Health and Family Welfare has issued the Standard Treatment Guidelines for Inguinal hernia treatment in children. Following are the major recommendations:
Case definition:
Inguinal hernia is a type of ventral hernia that occurs when an intra-abdominal structures, such as bowel or omentum, protrude through the open processus vaginalis through the inguinal canal.
INCIDENCE OF THE CONDITION IN OUR COUNTRY
Although the exact incidence of indirect inguinal hernia in infants and children is unknown, the reported incidence ranges from 1-5%. Sixty percent of hernias occur on the right side. Premature infants are at increased risk for inguinal hernia, with incidence rates of 2% in females and 7-30% in males. Inguinal hernias are much more common in males than in females. The male-to-female ratio is estimated to be 4-8:1. Premature infants are at an increased risk for inguinal hernia, with the incidence ranging from 7- 30%. Moreover, the associated risk of incarceration is more than 60% in this population.
DIFFERENTIAL DIAGNOSIS
Congenital Hydrocoele
Inguinal adenitis
Femoral adenitis
Psoas abscess
Saphenous varix
Retractile testis
Varicocele
Testicular tumor
Undescended testis
PREVENTION AND COUNSELING :
A high index of suspicion is required-especially in the high risk population of premature babies. If a child has developed a unilateral hernia, there is a potential risk of developing a hernia on the opposite side-this risk is higher in premature babies and infant girls. These families need to be counselled about signs and symptoms of these recurrences.
OPTIMAL DIAGNOSTIC CRITERIA, INVESTIGATIONS, TREATMENT & REFERRAL CRITERIA
diagnostic criteria: diagnosis is clinical.
1. History of a soft swelling in inguinal region. Gets larger when child cries, may disappear completely when the child is quietly lying down.
2. Examination: Soft, reducible mass in the inguinal area is diagnostic. Even in the absence of the mass at examination, a strong history is adequate for diagnosis.
Investigations:
No imaging studies are required. General tests towards anaesthesia fitness may be required ( haemoglobin, urine analysis).
Referral Criteria:
A strong clinical history and physical findings of inguinal hernia are indications for referral for surgery.
HISTORY
The child with an inguinal hernia presents with a bulge at the internal or external ring or within the scrotum. The parents typically provide the history of a visible swelling or bulge, commonly intermittent, in the inguinoscrotal region in boys and inguinolabial region in girls. Usually, a simple inguinal hernia in an infant is painless. The bulge commonly occurs after crying or straining and often resolves during the night while the baby is sleeping. If the family provides a history of a painful bulge in the inguinal region, one must suspect the presence of an incarcerated inguinal hernia. Patients with an incarcerated hernia generally present with a tender firm mass in the inguinal canal or scrotum. The child may be fussy, unwilling to feed, and inconsolably crying. The skin overlying the bulge may be edematous, erythematous, and discolored.
EXAMINATION
Physical examination of a child with an inguinal hernia typically reveals a palpable smooth mass originating from the external ring lateral to the pubic tubercle. The mass may only be noticeable after coughing or performing a Valsalva maneuver and it should be reduced easily.
Occasionally, the examining physician may feel the loops of intestine within the hernia sac. In girls, feeling the ovary in the hernia sac is not unusual; it is not infrequently confused with a lymph node in the groin region. In boys, palpation of both testicles is important to rule out an
undescended or retractile testicle.
Hernia and hydrocele: Transillumination has been advocated as a means of distinguishing between the presence of a sac filled with fluid in the scrotum (hydrocele) and the presence of bowel in the scrotal sac. However, in cases of inguinal hernia incarceration, transillumination may not be beneficial because any viscera that are distended and fluid-filled in the scrotum of a young infant may also transilluminate.
INVESTIGATIONS
No laboratory studies are needed in the assessment of a patient with a suspected inguinal hernia and/or hydrocele.
Ultrasonography: Its routine use is unnecessary. It is indicated when presentation and examination suggest a diagnosis other than hernia or hydrocele. An enlarged inguinal lymph node can mimic an incarcerated inguinal hernia.
Laparoscopy: Diagnostic laparoscopy may rarely be required for determining the presence of an inguinal hernia. It is used only in the following: a) assessment of contralateral hernia when one is being operated upon, and b) recurrent hernia after previous surgery.
TREATMENT
Congenital hernias are treated surgically with herniotomy. Surgical treatment can be either open or laparoscopic. Inguinal hernias do not spontaneously heal and must be surgically repaired because of the ever-present risk of incarceration. Repair is usually planned as an elective
procedure as soon as possible after diagnosis. If hernia is irreducible, ie cannot be easily pushed back into the abdomen, child needs to be
admitted and a manual reduction tried by an experienced pediatric surgeon. If successful, the operation is performed after 24-48 hours to allow local oedema to settle down. If reduction is unsuccessful, or if there is clinical evidence of inflammation (as evidenced by pain,
redness, edema of skin on hernia) emergency exploration and hernia repair is necessary.
Hydroceles without hernia in neonates:
This is the only exception in which surgical treatment may be delayed. Repair of hydroceles in neonates without the presence of hernia is typically delayed for 12 months because the connection with the peritoneal cavity (via the processus vaginalis) may be very small and may have already closed or be in the process of closing. If the hydorcoele persists after this observation period, operative repair is indicated and appropriate. Postpone the operation in the event of upper respiratory tract infection, otitis media, or significant rash in the groin.
FOLLOW UP
No specific limitations are indicated once the diagnosis of an inguinal hernia has been established; however, following operative repair, avoidance of major physical activity for 1 week is recommended. After that time, the patient is allowed to participate in physical activities (eg,sports, swimming, running). Children younger than 5 years are likely to recover extremely quickly from surgery; they are typically capable of returning to their normal level of activities within 24-48 hours of surgery.
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
a. Clinical Diagnosis:
Similar generic diagnostic criteria apply. A typical history and physical finding are adequate for diagnosis.
b. Investigations:
a. Investigations are not required other than for anaesthetic purposes.
b. Rarely, ultrasonography and diagnostic laparoscopy may be indicated
c. Treatment:
a. Inguinal hernia: Treatment is surgery -herniotomy operation that aims at ligating the patent processus vaginalis at the internal ring after reduction of contents into the abdomen.
b. Congenital hydrocoele: Treatment is deferred until the 2nd birthday as there is a 80% chance of spontaneous closure. Surgery is indicated if hydrocoele persists beyond the 2nd year and if it is rapidly growing is size.
c. All hernia and hydrocoele repairs in infants and children MUST be performed by a qualified pediatric surgeon.
Standard Operating procedure
a. In Patient : inpatient care is indicated if:
I. h/o incarceration or obstructions
II. neonate awaiting hernia repair
b. Out Patient
i. Outpatient care is adequate for diagnosis and follow up in most children
ii.Clinical evaluation usually sufficient to diagnose
c. Day Care
i. most hernia operations in children are done as day care procedures
Referral criteria:
A child with a hernia needs referral to a higher centre if:
1. neonatal age and anaesthesia facilities are inadequate
2. ex-premature baby who had prolonged ventilation
3. recurrent inguinal hernia
4. inguinal hernia with complications (incarceration, obstruction)
5. associated major morbidity-such as cardiac anomalies, lung disease, renal
disease, ascites.
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis:
Same as in situation1
Investigations:
Same as in situation1
additional tests for comorbid conditions such as pulmonary and cardiac
anomalies
Treatment:
a. principles of treatment are same as above
Standard Operating procedure
In Patient
i. criteria same as above
ii.all babies under 1 year of age need inpatient care after surgery-as there is an increased risk of apnoea in this subgroup.
iii. All children with comorbid problems-cardiac, respiratory or others, need inpatient care after surgery
b Out Patient
criteria same as above
c. Day Care
criteria same as above
Children who are above 1 year of age and in good health with no associated comorbid problems can be treated as day care procedures
Referral criteria:
No further referrals
WHO DOES WHAT? and TIMELINES
a. Doctor makes a clinical diagnosis, counsels the family and plans surgery- a pediatric surgeon performs the surgery
b. Nurse: assists surgeon in care of child during pre, intra and post operative course of the baby
c. Technician: assists medical and nursing teams in care of child during intra and post-operative periods.
RESOURCES REQUIRED FOR ONE PATIENT / PROCEDURE (PATIENT WEIGHT 60 KGS)
(Units to be specified for human resources, investigations, drugs and consumables and equipment. Quantity to also be specified)
Guideline Developed by Dr.Sanjay Rao
Dr.Vinay C
Dr. Zameer K
Consultant Pediatric Surgeons,
Narayana Hrudayalaya,
Bangalore
Case definition:
Inguinal hernia is a type of ventral hernia that occurs when an intra-abdominal structures, such as bowel or omentum, protrude through the open processus vaginalis through the inguinal canal.
INCIDENCE OF THE CONDITION IN OUR COUNTRY
Although the exact incidence of indirect inguinal hernia in infants and children is unknown, the reported incidence ranges from 1-5%. Sixty percent of hernias occur on the right side. Premature infants are at increased risk for inguinal hernia, with incidence rates of 2% in females and 7-30% in males. Inguinal hernias are much more common in males than in females. The male-to-female ratio is estimated to be 4-8:1. Premature infants are at an increased risk for inguinal hernia, with the incidence ranging from 7- 30%. Moreover, the associated risk of incarceration is more than 60% in this population.
DIFFERENTIAL DIAGNOSIS
Congenital Hydrocoele
Inguinal adenitis
Femoral adenitis
Psoas abscess
Saphenous varix
Retractile testis
Varicocele
Testicular tumor
Undescended testis
PREVENTION AND COUNSELING :
A high index of suspicion is required-especially in the high risk population of premature babies. If a child has developed a unilateral hernia, there is a potential risk of developing a hernia on the opposite side-this risk is higher in premature babies and infant girls. These families need to be counselled about signs and symptoms of these recurrences.
OPTIMAL DIAGNOSTIC CRITERIA, INVESTIGATIONS, TREATMENT & REFERRAL CRITERIA
diagnostic criteria: diagnosis is clinical.
1. History of a soft swelling in inguinal region. Gets larger when child cries, may disappear completely when the child is quietly lying down.
2. Examination: Soft, reducible mass in the inguinal area is diagnostic. Even in the absence of the mass at examination, a strong history is adequate for diagnosis.
Investigations:
No imaging studies are required. General tests towards anaesthesia fitness may be required ( haemoglobin, urine analysis).
Referral Criteria:
A strong clinical history and physical findings of inguinal hernia are indications for referral for surgery.
HISTORY
The child with an inguinal hernia presents with a bulge at the internal or external ring or within the scrotum. The parents typically provide the history of a visible swelling or bulge, commonly intermittent, in the inguinoscrotal region in boys and inguinolabial region in girls. Usually, a simple inguinal hernia in an infant is painless. The bulge commonly occurs after crying or straining and often resolves during the night while the baby is sleeping. If the family provides a history of a painful bulge in the inguinal region, one must suspect the presence of an incarcerated inguinal hernia. Patients with an incarcerated hernia generally present with a tender firm mass in the inguinal canal or scrotum. The child may be fussy, unwilling to feed, and inconsolably crying. The skin overlying the bulge may be edematous, erythematous, and discolored.
EXAMINATION
Physical examination of a child with an inguinal hernia typically reveals a palpable smooth mass originating from the external ring lateral to the pubic tubercle. The mass may only be noticeable after coughing or performing a Valsalva maneuver and it should be reduced easily.
Occasionally, the examining physician may feel the loops of intestine within the hernia sac. In girls, feeling the ovary in the hernia sac is not unusual; it is not infrequently confused with a lymph node in the groin region. In boys, palpation of both testicles is important to rule out an
undescended or retractile testicle.
Hernia and hydrocele: Transillumination has been advocated as a means of distinguishing between the presence of a sac filled with fluid in the scrotum (hydrocele) and the presence of bowel in the scrotal sac. However, in cases of inguinal hernia incarceration, transillumination may not be beneficial because any viscera that are distended and fluid-filled in the scrotum of a young infant may also transilluminate.
INVESTIGATIONS
No laboratory studies are needed in the assessment of a patient with a suspected inguinal hernia and/or hydrocele.
Ultrasonography: Its routine use is unnecessary. It is indicated when presentation and examination suggest a diagnosis other than hernia or hydrocele. An enlarged inguinal lymph node can mimic an incarcerated inguinal hernia.
Laparoscopy: Diagnostic laparoscopy may rarely be required for determining the presence of an inguinal hernia. It is used only in the following: a) assessment of contralateral hernia when one is being operated upon, and b) recurrent hernia after previous surgery.
TREATMENT
Congenital hernias are treated surgically with herniotomy. Surgical treatment can be either open or laparoscopic. Inguinal hernias do not spontaneously heal and must be surgically repaired because of the ever-present risk of incarceration. Repair is usually planned as an elective
procedure as soon as possible after diagnosis. If hernia is irreducible, ie cannot be easily pushed back into the abdomen, child needs to be
admitted and a manual reduction tried by an experienced pediatric surgeon. If successful, the operation is performed after 24-48 hours to allow local oedema to settle down. If reduction is unsuccessful, or if there is clinical evidence of inflammation (as evidenced by pain,
redness, edema of skin on hernia) emergency exploration and hernia repair is necessary.
Hydroceles without hernia in neonates:
This is the only exception in which surgical treatment may be delayed. Repair of hydroceles in neonates without the presence of hernia is typically delayed for 12 months because the connection with the peritoneal cavity (via the processus vaginalis) may be very small and may have already closed or be in the process of closing. If the hydorcoele persists after this observation period, operative repair is indicated and appropriate. Postpone the operation in the event of upper respiratory tract infection, otitis media, or significant rash in the groin.
FOLLOW UP
No specific limitations are indicated once the diagnosis of an inguinal hernia has been established; however, following operative repair, avoidance of major physical activity for 1 week is recommended. After that time, the patient is allowed to participate in physical activities (eg,sports, swimming, running). Children younger than 5 years are likely to recover extremely quickly from surgery; they are typically capable of returning to their normal level of activities within 24-48 hours of surgery.
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
a. Clinical Diagnosis:
Similar generic diagnostic criteria apply. A typical history and physical finding are adequate for diagnosis.
b. Investigations:
a. Investigations are not required other than for anaesthetic purposes.
b. Rarely, ultrasonography and diagnostic laparoscopy may be indicated
c. Treatment:
a. Inguinal hernia: Treatment is surgery -herniotomy operation that aims at ligating the patent processus vaginalis at the internal ring after reduction of contents into the abdomen.
b. Congenital hydrocoele: Treatment is deferred until the 2nd birthday as there is a 80% chance of spontaneous closure. Surgery is indicated if hydrocoele persists beyond the 2nd year and if it is rapidly growing is size.
c. All hernia and hydrocoele repairs in infants and children MUST be performed by a qualified pediatric surgeon.
Standard Operating procedure
a. In Patient : inpatient care is indicated if:
I. h/o incarceration or obstructions
II. neonate awaiting hernia repair
b. Out Patient
i. Outpatient care is adequate for diagnosis and follow up in most children
ii.Clinical evaluation usually sufficient to diagnose
c. Day Care
i. most hernia operations in children are done as day care procedures
Referral criteria:
A child with a hernia needs referral to a higher centre if:
1. neonatal age and anaesthesia facilities are inadequate
2. ex-premature baby who had prolonged ventilation
3. recurrent inguinal hernia
4. inguinal hernia with complications (incarceration, obstruction)
5. associated major morbidity-such as cardiac anomalies, lung disease, renal
disease, ascites.
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis:
Same as in situation1
Investigations:
Same as in situation1
additional tests for comorbid conditions such as pulmonary and cardiac
anomalies
Treatment:
a. principles of treatment are same as above
Standard Operating procedure
In Patient
i. criteria same as above
ii.all babies under 1 year of age need inpatient care after surgery-as there is an increased risk of apnoea in this subgroup.
iii. All children with comorbid problems-cardiac, respiratory or others, need inpatient care after surgery
b Out Patient
criteria same as above
c. Day Care
criteria same as above
Children who are above 1 year of age and in good health with no associated comorbid problems can be treated as day care procedures
Referral criteria:
No further referrals
WHO DOES WHAT? and TIMELINES
a. Doctor makes a clinical diagnosis, counsels the family and plans surgery- a pediatric surgeon performs the surgery
b. Nurse: assists surgeon in care of child during pre, intra and post operative course of the baby
c. Technician: assists medical and nursing teams in care of child during intra and post-operative periods.
RESOURCES REQUIRED FOR ONE PATIENT / PROCEDURE (PATIENT WEIGHT 60 KGS)
(Units to be specified for human resources, investigations, drugs and consumables and equipment. Quantity to also be specified)
| Situation | Human Resources | Drugs & Consumables | Equipment |
| 1 | · Pediatric Surgeon · Pediatrician · Pediatric Nurse · Lab. Technician | · I.V. Glucose/ Fluids · I.V. cannula · I.V. Set · anesthetic drugs, disposables · antibiotic prophylaxis | · Radiant Warmer · Saturation monitor · Basic Lab · Child friendly OT |
| 2 | · Pediatric surgeon · Pediatrician · Pediatric anaesthesist · Pediatric Nurse | · I.V. Glucose/ Fluids · I.V. cannula · I.V. Set · anesthetic drugs, disposables · antibiotic prophylaxis | · ICU · Pediatric O.T. |
Guideline Developed by Dr.Sanjay Rao
Dr.Vinay C
Dr. Zameer K
Consultant Pediatric Surgeons,
Narayana Hrudayalaya,
Bangalore
Group Head Coordinator of Development Team
Dr Ashley J D'cruz
Narayana Hurdayalaya
Bangalore
Congenital HydrocoeleFemoral adenitisInguinal adenitisInguinal hernia in childrenlaparoscopyPREVENTION AND COUNSELINGPsoas abscessRetractile testisSaphenous varixTesticular tumorUltrasonographyUndescended testisVaricocele
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd