- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Infective Endophthalmitis - Standard Treatment Guidelines
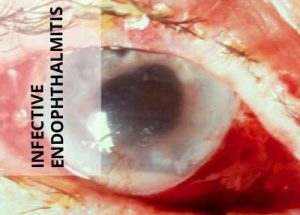
Exogenous Endophthalmitis is a devastating complication, usually following intraocular surgery or open globe injury. Rarely, a hematogenous dissemination into the eye from a distant focus of injection within the body may be a cause and this form is termed as endogenous endophthalmitis in this condition, the internal structure of the eye are invaded by replicating microorganisms, resulting in an inflammatory response that ultimately may involve all tissues of the eye. This serious condition can be effectively treated if diagnosed early and treated comprehensively.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Infective Endophthalmitis. Following are the major recommendations :
Case definition:
Endophthalmitis is defined as a serious intraocular inflammation resulting from infection of the vitreous cavity. Exogenous endophthalmitis occurs when infective organisms gain entry into the eye by direct inoculation, such as from intraocular surgery, intravitreal injections, penetrating trauma, or contiguous spread from adjacent tissues. Endogenous endophthalmitis occurs when infectious agents are hematogenously disseminated into the eye from a distant focus of infection. Initial intraocular signs and symptoms may include decreased visual acuity, afferent pupillary defect, pain, hypopyon, fibrinoid anterior chamber response, corneal edema, corneal/wound infiltrate, vitreous inflammation, retinitis, and/or retinal periphlebitis. External signs of inflammation, such as ciliary injection, chemosis, and lid edema, may be present. If the infection has spread to orbit, restriction of extraocular motility and proptosis may occur.
Incidence of The Condition In Our Country
The national survey on blindness and visual outcome after cataract surgery in 2001, carried out by the ministry of health, Government of India, found an incidence of 0.6%. In a study conducted by a major tertiary care centre, the incidence of post operative endophthalmitis was found to be 0.09%. Traumatic endophthalmitis accounts for approximately 7% of open globe injuries and nearly a quarter of all endophthalmitis cases. Endogenous endophthalmits accounts for 2.6% of all culture positive endophthalmitis.
Differential Diagnosis
The following are the differential diagnosis
a) Sterile uveitis
b) Phacoanaphylactic endophthtalmitis
c) Sympathetic ophthalmia
Sterile inflammation may result from retained intraocular foreign material like cotton fibers, from toxic reaction to drugs or irrigating fluids, from operative trauma, from exacerbation of preexisting uveitis, and from other conditions like phacoanaphylactic endophthalmitis and sympathetic ophthalmia. Post trauma or post cataract surgery severe inflammation with true hypopyon can result from retained lens fragments. Ultrasonography may be helpful in establishing the diagnosis. The clinical presentation depends on cause, therefore the history may be helpful, and should include the details of recent surgery, allergy history and uveitis history.
Prevention And Counseling
The mainstay of prevention of post operative endophthalmitis is maintenance of strict surgical asepsis during any intraocular surgery. The ocular surface and adnexa are the primary sources of microbes in culture positive cases of post operative endophthalmitis. The use of topical 5% povidine iodine solution in the conjunctival fornices before performing intraocular surgery reduces the bacterial load and decreases the incidence of this condition. The second line of prevention is use of broad spectrum and bactericidial topical / periocular/ intracameral antibiotics. Numerous surgical studies have confirmed that prophylactic antibiotics are maximally effective preoperatively and less effective postoperatively in preventing endophthalmits. In case of post operative endophthalmitis, prompt referral to a tertiary care centre in case of slightest doubt is mandatory. Investigations have to be immediately performed to rule out any intra ocular foreign body.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis :
The diagnosis of endophthalmitis is based on the clinical presentation, be it postoperative, post-trauma or endogenous. Any eye with inflammation greater than the usual postoperative or post-trauma clinical course should be suspected of having endophthalmitis. Symptomatically, typically the patient notes a sudden increase in pain and
decrease in vision which may manifest after a variable time period after an intraocular surgery or open globe injury. Examination demonstrates conjunctival chemosis and increased injection. The upper lid becomes edematous and the cornea shows variable degree of edema. The anterior chamber shows increased flare and cells, and hypopyon is often present in the inferior angle. Fundus view is obscured by focal or diffuse vitritis which manifests as a yellow glow. In more extreme cases the anterior chamber is filled with exudates and the cornea is white. If the infection has spread to orbit, restriction of extraocular motility and proptosis may occur.
Investigations:
i) When measuring visual acuity, the technique of differentiating light perception from hand motions vision is most important, since this is a major factor in determining candidates most likely to benefit from vitrectomy in postoperative endophthalmitis. Hand motions vision should be determined no closer than 2 feet from the patient with light illumination originating from behind the patient.
ii) A diligent clinical examination with slit lamp biomicroscopy should be done to look for certain risk factors which influence the management. These include wound leak or dehiscence, suture abscess and vitreous incarceration in the wound in postoperative endophthalmitis. Additionally, presence of intraocular foreign body and lens disruption should be recognized in post-trauma endophthalmitis.
iii) Ultrasound evaluation of the globe should be performed if significant media opacification prevents an adequate view of the fundus. Findings consistent with endophthalmitis include dispersed vitreous opacities from associated vitritis and in advanced cases, chorioretinal thickening. The ultrasound examination should rule out associated retinal or choroidal detachment, dislocated lens material, or intraocular foreign bodies.
iv) Ocular samples should be obtained for microbial identification. As there are no significant differences in yield of positive cultures among the needle tap, vitreous biopsy, or pars plana vitrectomy techniques, the surgeon may decide the best possible sampling method based on the resources available. Retrobulbar anesthesia may be necessary but must be administered cautiously in the presence of recent ocular surgical wound or open globe injury. The eye is surgically prepared with povidone iodine 5% solution and rinsed thoroughly with sterile balanced salt solution or normal saline to remove residual antiseptic from the ocular surface. A surgical drape, lid speculum and operating microscope may be used. A 30 gauge needle attached to a tuberculin syringe is inserted through the limbus into the anterior chamber and an aqueous specimen is aspirated without collapsing the anterior chamber. A quantity of approximately 0.1ml can usually be obtained. A vitreous specimen may be obtained either by vitreous needle tap or by vitreous biopsy with a vitreous cutter. After conjunctival incision, a vitrectomy probe attached to a tuberculin syringe is inserted into the vitreous cavity through a sclerotomy incision placed 3mm posterior to the limbus. Approximately 0.1-0.3ml of vitreous is removed from the anterior vitreous cavity by using the automated cutting mechanism of the probe and slow, manual aspiration into the syringe. The alternative method, vitreous needle tap, is performed by inserting a 27 to 23 gauge needle attached to a tuberculin syringe into the vitreous cavity through the pars plana, and slowly aspirating a similar volume of fluid vitreous. Samples collected should be sent immediately for Gram and KOH staining. It is ideal to inoculate the samples for culture (aerobic, anaerobic and fungal) within minutes of obtaining them to maximize the culture yield.
Treatment:
i) Postoperative endophthalmitis : the main treatment is in the form of intravitreal antibiotics since it is the best way to achieve therapeutic concentration in the eye. An empirical treatment with broadspectum antibiotics is initiated concomitantly with the ocular fluid biopsy or core vitrectomy. The recommended combinations of antibiotics for empirical therapy are Vancomycin 1.0mg/0/1ml and Ceftazidime 2.25mg/0.1ml. Amikacin 400 microgm/0.1ml can be considered in exchange for ceftazidime in beta-lactam sensitive patients. In cases of suspected fungal endophthalmitis intravitreal antifungal agents should be administered.
In addition to eradication of viable organisms from the eye and sterilization of the vitreous cavity, control of intraocular inflammation is an important therapeutic goal. Inflammation can increase even when microbes are no longer viable. Corticosteroid administration at the appropriate time - no matter what route is chosen - is to be administered to reduce the ocular inflammation and maintain the structural integrity of the globe.
Immediate vitrectomy should be reserved for severe endophthalmitis with a presenting vision of perception of light. Such cases carry a significant, threefold improved chance of obtaining 6/12 vision in comparison to vitreous tap or biopsy according to endophthalmitis vitrectomy study. However, the procedure is not without risks such as vitreous haemorrhage, retinal tears and retinal detachment. Hence a limited vitrectomy of the core of the vitreous is advocated by various investigators. Improved viewing systems and instrumentations have enabled surgeons to perform complete vitrectomies with claims of better visual results and fewer complications. It is highly recommended to choose the right amount of vitreous debulking depending on the visibility of the fundus structures and severity of the inflammation. The best way to avoid complications is to keep intraocular pressure at a constant level during the entire procedure, thereby preventing hypotony.
Post surgery management includes use of topical antibiotics based on the culture sensitivity. In situations where no organisms are grown on culture, a combination of antibiotic or a broad spectrum antibiotic should be chosen to cover both the gram negative and gram positive spectrum of causative organisms. Role of systemic antibiotics are debatable considering its low intraocular bioavailability.
After initial treatment of endophthalmitis a fraction of patients would require further treatment, mainly for worsening ocular infection or complication from the initial procedure. It typically requires more than 48hrs to observe an improvement in the clinical appearance after initial treatment. But one needs to keep in mind that the treated eyes look somewhat worse 1 day after treatment before improving subsequently.
ii) Traumatic endophthalmitis : When the diagnosis of traumatic endophthalmitis is established, aqueous and vitreous specimen should be obtained for culture and Gram stain. Intravitreal injection with appropriate antimicrobial agent may be given as an initial treatment. But the guidelines for postoperative endophthalmitis treatment may not be applicable for traumatic endophthalmitis because of the diversity of the organisms encountered. Early closure of the wound, removal of foreign body and Vitrectomy in patients with severe vitritis should be the standard of care in all cases of traumatic endophthalmitis where the injury involves a rupture of ocular coats, or rupture of lens. Patients who do not respond after 48hrs or rapidly deteriorate in the first 24hrs following intravitreal antibiotics should also be treated with vitrectomy. Just like postoperative endophthalmitis, the exact role of systemic antimicrobial therapy for traumatic endophthalmitis is unclear.
Endogenous endophthalmitis: In contrast to postoperative endophthalmitis and traumatic endophthalmitis, systemic antibiotics are central to treatment of the endogenous endophthalmitis, since the source of infection is often remote to eyes. A detailed systemic workup including a general physical examination with special attention to the heart, skin and extremities should be carried out to look for the source of origin of the infection. When the source of infection is not apparent, special diagnostic studies like echocardiogram, abdominal ultrasonography, culture of blood and urine should be done. Cases of endogenous endophthalmitis with mild inflammation (e.g., focal metastatic abscesses in the anterior or posterior segment) may be treated initially with topical and systemic therapy, using nonocular cultures to guide treatment. Intravitreal antibiotic injection may be indicated if: 1) the inflammatory focus is in the anterior segment, and the eye is aphakic, or there is a dehiscence in the posterior capsule; or 2) the inflammatory focus is in the posterior segment, and there is significant vitritis. If no improvement is seen within a reasonable length of time or if nonocular cultures are negative, biopsy is indicated. Unlike cases of postoperative or posttraumatic endophthalmitis, the vitreous may not be the principal site of infection in endogenous endophthalmitis. For this reason, biopsies should be taken from the area that is the primary site of ocular inoculation/inflammation.
List of commonly used antibiotics with recommended doses:
| Antibiotic | Topical | Subconjunctival | Intravitreal |
| Amikacin | 20mg/ml | 40mg/ml | 400micgm |
| Amphotericin B | 0.15-0.5% | - | 5-10micgm |
| Ampicillin | 50mg/ml | 100mg | 5mg |
| Cefazoline | 50mg/ml | 100mg | 2.25mg |
| Ceftazidime | 50mg/ml | 100mg | 2.25mg |
| Ciprofloxacin | 0.30% | 1mg | 100-500micgm |
| Clindamycin | - | 30mg | 250micgm |
| Fluconazole | 0.20% | 2%-1ml | 10-100micgm |
| Gatifloxacin | 0.30% | - | 400micgm |
| Gentamicin | 10-20mg/ml | 20mg | 200micgm |
| Levofloxacin | 0.50% | - | 625micgm |
| Miconazole | 10mg/ml | 5mg | 25micgm |
| Moxifloxacin | 0.50% | - | 400micgm |
| Tobramycin | 8-15mg/ml | 20mg | 200micgm |
| Vancomycin | 50mg/ml | 25mg | 1mg |
| Voriconazole | 1-2% | - | 100micgm |
Standard Operating procedure
In Patient
All patients with endophthalmitis should be admitted and treated as in patients
Out Patient
Not applicable
Day Care
Not applicable
Referral criteria:
i) Postoperative endophthalmitis with presenting vision of light perceptions.
ii) Severe postoperative endophthalmitis
iii) Traumatic endophthalmitis with lens rupture and intraocular foreign body.
iv) Endogenous endophthalmitis worsening in spite of maximum treatment
v) Endophthalmitis in the only seeing eye
vi) Paediatric patients needing general anaesthesia
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis:
The surgeon at the tertiary care center should elicit the history of the disease afresh to plug the missing links if any, especially in endogenous endophthalmitis. Postoperative and traumatic endophthalmitis history is generally straight forward. A detailed treatment history and the culture results if any should be noted. In culture negative cases fresh investigations should be initiated to rule out phacoanphylactic endophthalmitis or retained intraocular foreign body.
Investigations:
Meticulous ultrasonogram of the eye may detect retained lens matter. Compuerised tomography may detect occult intraocular foreign bodies in traumatic endophthalmitis. Special investigations like polymerase chain reaction of the vitreous or aqueous samples may be an useful additional diagnostic tool in culture negative cases. A repeat smear and culture of ocular fluids is mandated. The commonly used stains and culture media are mentioned below.
| Presumed organisms | Stain | Media |
| Aerobic bacteria | Gram Giemsa | Blood agar Chocolate agar Thioglycolate broth |
| Anaerobic bacteria | Gram | Anaerobic blood agar Thioglycolate broth |
| Fungi | 10%KOH Gram Calcofluor white | Blood agar Saboraud dextrose agar Brain heart infusion |
Treatment:
The culture sensitivity results help in choosing appropriate antibiotics for treatment.
1.Vancomycin and ceftazidime with or without dexamethasone stand as the preferred combinations of intravitreal drugs if no organisms are isolated.
2.A combination of vancomycin with amikacin is advocated as the empirical treatment in traumatic endophthalmitis.
3.In Soil contaminated foreign body injuries where bacillus caerus is suspected, combination of gentamicin with clindamicin in an option.
4. Pars plana vitrectomy remains the treatment of choice in severe endophthalmitis and in cases where the disease progression is noted in spite of the initial antibiotic treatment.
The first technical problem that confronts the surgeon is placement of the infusion cannula. Because the media is almost always too cloudy for the surgeon to be able to visualize a pars plana port, this infusion cannot be used for the initial stages of the operation. Because the incision and placement of the infusion port are easier in a firm eye, it is often worthwhile placing an inferotemporal port with sutures, reserving its use for later in the procedure, once the location of the tip in the vitreous cavity can be verified.
The presence of the crystalline lens or a pseudophakos will determine placement of the canula (3.5mm from limbus in pseudophacos, 4mm in phakic eyes). If light is not needed during the initial portion of the procedure, a bent needle or other blunt infusion canula can be positioned in the center of the pupillary space, where its position can be monitored. This infusion can be turned on at this stage so that the incision through the pars plana for the cutting instrument may be made in a firm eye. The anterior chamber often contains significant amounts of fibrin and hypopyon. Because the cornea invariably has some combination of epithelial edema, folds, and cells deposited on the posterior surface, the iris and central anterior vitreous are often impossible to visualize adequately. Initial incisions may be made in the limbus at approximately the 9.30 and 2.30 clock positions, modifying the location as necessary depending on the condition of the previous surgical wound and on the presence of a filtering bleb. Fluid is infused into the anterior chamber as inflammatory debris is removed with the suction and cutting instrument. If an inflammatory membrane extends over the iris surface and the lens, a bent needle can be used to gently peel it off the surface. The vitrectomy is now progressively carried posteriorly. The vitreous removal is performed initially in the center of the vitreous cavity. Pockets of more heavily infiltrated vitreous are sometimes located; in the aphakic eye, peripheral depression may be used to bring these into view. Aggressive removal of all infiltrated vitreous in the basal area should not be attempted because this often results in retinal tears. The presence of a posterior vitreous detachment, on the other hand, allows more complete vitreous removal. If the vitreous is still attached, a judgment must be made about the amount of vitreous to be removed. The cutting of vitreous adjacent to inflamed or necrotic retina will often cause retinal breaks; these are difficult to seal and may result in failure of the case. In eyes with posterior vitreous detachment, a white mound of inflammatory debris may be visible over the posterior pole. This should be approached with care and may be gently aspirated into the cutting port. If the mound proves to be solid and adherent, small amounts can usually be removed, but in most cases it is unwise to attempt to remove large portions. In some instances the material is flocculent and equivalent to an unorganized hypopyon; this can be gently sucked up with vacuum techniques. The procedure is completed by closing all incisions in a watertight manner and injecting intraocular antibiotics. After closure of the conjunctival incisions, subconjunctival antibiotics are often injected.
Standard Operating procedure
In Patient
i) Postoperative endophthalmitis
ii) Traumatic endophthalmitis
iii) Endogenous endophthamitis
Out Patient
Not applicable
C. Day Care
Not applicable
Referral criteria:
Not applicable
WHO DOES WHAT? And TIMELINES
Doctor
- Elicits patient history and performs clinical Examination
- Collects ocular fluid sample and inoculates for smear and culture
- Maintains medical records
- Plans the appropriate treatment
- Performs surgery
- Monitors, publishes and reports to department of health any emergence of drug resistant strains of microbes.
Nurse
- Maintains separate inpatient and outpatient record
- Prepares the patient for operative procedures
- Monitors the inpatients to ensure compliance
Technician
- Prepares slide, media for smear and culture
- Maintains lab records
- Performs ultrasonography when necessary and maintains records
Resources Required
| Situation | HUMAN RESOURCES | INVESTIGATION | DRUGS & CONSUMABLES | EQUIPMENT |
| 1) Secondary level | 1)Ophthalmologist - 1 2)OP Nurse – 1 3)Refraction nurse - 1(shared ) | 1)Smear test 2)Gram stain microscopy 3)KOH smear | 1)Antibiotics eye drops 2)Antifungal eye drops 3)Systemic antibiotics steroids and anti fungals 4) Mydriatic clyclopigic 5) Needles and syringes 6) Basic stains | 1)Slit lamp - biomicroscope -1 2)Light microscope -1 3)Disposable needles 4)Tuberculin syringe- 5 5)Glass slide - 1 6)Basic stains - 1 |
| 2) Tertiary level | 1) Retina specialist - 1 2)Refraction nurse - 1(shared ) 3)OP Nurse - 1 4) Lab technician - 1 5)Scrub nurse - 1 6)OT nurse - 1 7)Ward nurse -1 8) Counsellor - 1 | 1)Smear test 2)Culture medium 3)Antibiotic sensitivity plates 4)Corneal biopsy 5)PCR | 1)Antibiotics eye drops 2)Antifungal eye drops 3)Systemic antibiotics and anti fungal 4) Topical and systemic steroids 5) Mydriatic and cyclopigic 6) Irrigating solutions 7) Needles and syringes 8) Basic stains | 1)Slit lamp - biomicroscope -1 2)Light microscop -1 3)Ultrasonogram -1 4)Vitrectomy equipment -1 5)OT microsurgical instruments -1 6)PCR instruments -1 |
Guidelines by The Ministry of Health and Family Welfare :
Dr. Venkatesh Prajna Chief- Dept of Medical Education, Aravind Eye Hospitals, Madurai

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd