- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Incontinence after Prostate Treatment: AUA releases 2019 Guideline
American Urological Association(AUA) has released its latest 2019 Guideline on the management of Incontinence after Prostate Treatment.
Urinary incontinence after prostate treatment (IPT) is a clinically significant condition that causes a high degree of patient distress. It is one of the few urologic diseases that is iatrogenic, and, therefore, predictable and perhaps preventable. American Urological Association(AUA) has underlined multiple treatments that exist for patients with IPT are discussed and evaluated, including physical therapy, medications, and surgery. The American Urological Association(AUA) panel conducted searches in Ovid MEDLINE (from 2000 to December 21st, 2017), Cochrane Central Register of Controlled Trials (from 2000 to December 21st, 2017) and Cochrane Databases of Systematic Reviews (from 2000 to December 21st, 2017).
Following are the major recommendations of American Urological Association(AUA):
Pre-Treatment
1. Clinicians should inform patients undergoing radical prostatectomy of all known factors that could affect continence. (Moderate Recommendation; Evidence Level: Grade B)
2. Clinicians should counsel patients regarding the risk of sexual arousal incontinence and climacturia following radical prostatectomy. (Strong Recommendation; Evidence Level: Grade B)
3. Clinicians should inform patients undergoing radical prostatectomy that incontinence is expected in the short-term and generally improves to near baseline by 12 months after surgery but may persist and require treatment. (Strong Recommendation; Evidence Level: Grade A)
4. Prior to radical prostatectomy, patients may be offered pelvic floor muscle exercises or pelvic floor muscle training. (Conditional Recommendation; Evidence Level: Grade C)
5. Patients undergoing transurethral resection of the prostate after radiation therapy or radical prostatectomy after radiation therapy should be informed of the high rate of urinary incontinence following these procedures. (Moderate Recommendation; Evidence Level: Grade C)
Post-Prostate Treatment
6. In patients who have undergone radical prostatectomy, clinicians should offer pelvic floor muscle exercises or pelvic floor muscle training in the immediate post-operative period. (Moderate Recommendation; Evidence Level: Grade B)
7. In patients with bothersome stress urinary incontinence after prostate treatment, surgery may be considered as early as six months if incontinence is not improving despite conservative therapy. (Conditional Recommendation; Evidence Level: Grade C)
8. In patients with bothersome stress urinary incontinence after prostate treatment, despite conservative therapy, surgical treatment should be offered at one-year post-prostate treatment. (Strong Recommendation; Evidence Level: Grade B)
Evaluation of Incontinence after Prostate Treatment
9. Clinicians should evaluate patients with incontinence after prostate treatment with history, physical exam, and appropriate diagnostic modalities to categorize type and severity of incontinence and degree of bother. (Clinical Principle)
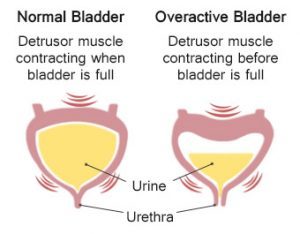
10. Patients with urgency urinary incontinence or urgency predominant mixed urinary incontinence should be offered treatment options per the American Urological Association Overactive Bladder guideline. (Clinical Principle)
11. Prior to surgical intervention for stress urinary incontinence, stress urinary incontinence should be confirmed by history, physical exam, or ancillary testing. (Clinical Principle)
12. Patients with incontinence after prostate treatment should be informed of management options for their incontinence, including surgical and non-surgical options. (Clinical Principle)
13. In patients with incontinence after prostate treatment, physicians should discuss risk, benefits, and expectations of different treatments using the shared decision-making model. (Clinical Principle)
14. Prior to surgical intervention for stress urinary incontinence, cystourethroscopy should be performed to assess for urethral and bladder pathology that may affect outcomes of surgery. (Expert Opinion)
15. Clinicians may perform urodynamic testing in a patient prior to surgical intervention for stress urinary incontinence in cases where it may facilitate diagnosis or counseling. (Conditional Recommendation; Evidence Level: Grade C)
Treatment Options
16. In patients seeking treatment for incontinence after radical prostatectomy, pelvic floor muscle exercises or pelvic floor muscle training should be offered. (Moderate Recommendation; Evidence Level: Grade B)
17. Artificial urinary sphincter should be considered for patients with bothersome stress urinary incontinence after prostate treatment. (Strong Recommendation; Evidence Level: Grade B)
18. Prior to implantation of artificial urinary sphincter, clinicians should ensure that patients have adequate physical and cognitive abilities to operate the device. (Clinical Principle)
19. In the patient who selects artificial urinary sphincter, a single cuff perineal approach is preferred. (Moderate Recommendation; Evidence Level: Grade C)
20. Male slings should be considered as treatment options for mild to moderate stress urinary incontinence after prostate treatment. (Moderate Recommendation; Evidence Level: Grade B)
21. Male slings should not be routinely performed in patients with severe stress incontinence. (Moderate Recommendation; Evidence Level: Grade C)
22. Adjustable balloon devices may be offered to patients with mild stress urinary incontinence after prostate treatment. (Moderate Recommendation; Evidence Level: Grade B)
23. Surgical management of stress urinary incontinence after treatment of benign prostatic hyperplasia is the same as that for patients after radical prostatectomy. (Moderate Recommendation; Evidence Level: Grade C)
24. In men with stress urinary incontinence after primary, adjuvant, or salvage radiotherapy who are seeking surgical management, artificial urinary sphincter is preferred over male slings or adjustable balloons. (Moderate Recommendation; Evidence Level: Grade C)
25. Patients with incontinence after prostate treatment should be counseled that efficacy is low and cure is rare with urethral bulking agents. (Strong Recommendation; Evidence Level: Grade B)
26. Other potential treatments for incontinence after prostate treatment should be considered investigational, and patients should be counseled accordingly. (Expert Opinion)
Complications after Surgery
27. Patients should be counseled that artificial urinary sphincter will likely lose effectiveness over time, and reoperations are common. (Strong Recommendation; Evidence Level: Grade B)
28. In patients with persistent or recurrent urinary incontinence after artificial urinary sphincter or sling, clinicians should again perform history, physical examination, and/or other investigations to determine the cause of incontinence. (Clinical Principle)
29. In patients with persistent or recurrent stress urinary incontinence after sling, an artificial urinary sphincter is recommended. (Moderate Recommendation; Evidence Level: Grade C)
30. In patients with persistent or recurrent stress urinary incontinence after artificial urinary sphincter, revision should be considered. (Strong Recommendation; Evidence Level: Grade B)
Special Situations
31. In a patient presenting with infection or erosion of an artificial urinary sphincter or sling, explantation should be performed and reimplantation should be delayed. (Clinical Principle)
32. A urinary diversion can be considered in patients who are unable to obtain long-term quality of life after incontinence after prostate treatment and who are appropriately motivated and counseled. (Expert Opinion)
33. In a patient with bothersome climacturia, treatment may be offered. (Conditional Recommendation; Evidence Level: Grade C)
34. Patients with stress urinary incontinence following urethral reconstructive surgery may be offered artificial urinary sphincter and should be counseled that complications rates are higher. (Conditional Recommendation; Evidence Level: Grade C)
35. In patients with incontinence after prostate treatment and erectile dysfunction, a concomitant or staged procedure may be offered. (Conditional Recommendation; Evidence Level: Grade C)
36. Patients with symptomatic vesicourethral anastomotic stenosis or bladder neck contracture should be treated prior to surgery for incontinence after prostate treatment. (Clinical Principle).
For more details click on the link: www.auanet.org

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd