- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Imaging of acute traumatic aortic injury
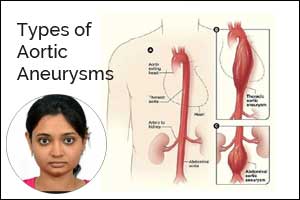
Contrast-enhanced CT has become the modality of choice in the diagnosis of acute traumatic aortic injuries (ATAIs) in recent times. Advancements in endovascular repair techniques demand precise diagnosis, grading, detection of the true & false lumen (in aortic dissection) and assessment of severity. High mortality and morbidity associated with such injuries require rapid imaging and treatment. Also, in nontraumatic atherosclerotic aneurysms treated with endovascular therapy, follow-up CT is needed in ATAIs to assess the quality of pseudoaneurysm exclusion and to evaluate for post-intervention complications.
The most common location for imaged acute traumatic aortic injury in the setting of blunt trauma is at the aortic isthmus, just distal to the origin of the left subclavian artery, due to the relatively fixed position of the aorta at the site of the ligamentumarteriosum.
Types of injury- penetrating/blunt
Radiograph sign- widening of the mediastinum highly suspicious for a mediastinal hematoma in a post-trauma setting.
Indirect sign- periaortic hematoma
Direct signs- vessel wall disruption with or without focal out pouching, aortic wall thickening, high attenuation within the aortic wall
Intimal calcification displacement may be seen in case of aortic dissection. (Can be seen on a non- contrast CT itself).
True versus false lumen on CT: features in favour of false lumen
- Flow or occluded by thrombus (chronic).
- Delayed enhancement
- Wedges around true lumen (beak-sign)
- Collageneous media-remnants (cobweb sign)
- Larger than true lumen
CT mimics and pitfalls
- Vascular pulsation artefact
- Respiratory motion
- Streak artefact due to dense contrast in SVC
- Flow artefact in setting of low cardiac output
Corrected by
ECG Gating to minimize pulsation
- Saline chaser following contrast injection or longer delay time
- Arms over head instead of by the side
- Knowledge of potential anatomical variants like ductus diverticulum and aortic spindle.
- Mercedes Benz sign
Triple-barreled aortic dissection/Three intimal flaps
Intimo-intimal intussusception: a rare clinical form of aortic dissection!
New concepts-
- Use of reformatted images with a 5-mm section thickness, non-contrast with use of a narrow window is more helpful than thin images to detect intramural hematoma.
- Following items should be included in the radiology report: Stanford classification; maximum aortic diameter; maximum hematoma thickness; presence or absence of focal contrast enhancement (ie, intramural blood pool or ulcer-like projection); ulcer-like projection diameter and depth); and presence or absence of pleural effusion, pericardial effusion, and periaortic hematoma.
- Current guidelines in the modern era of MDCT, state conventional angiography is no longer indicated for stable patients with a mediastinal hematoma in absence of direct signs of aortic injury.
Dr. Niharika Prasad,
The author is MD (Radiodiagnosis) and is Senior Resident, Dept of Radiology in All India Institute of Medical Sciences, AIIMS Patna. She is a member Editorial Board, Radiology at Specialty Medical Dialogues.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd