- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
ILUMIEN III OPTIMIZE PCI trial-Guiding coronary stent implantation
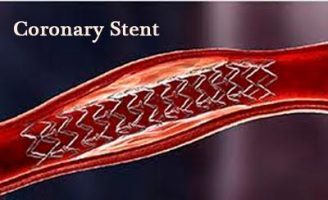
Although percutaneous coronary intervention (PCI) is most commonly guided by angiography alone, results from a new study investigating adjunctive imaging modalities showed that the use of a novel optical coherence tomography (OCT)-based stent sizing strategy results in similar minimal stent area (MSA) compared to intravascular ultrasound (IVUS)-guided PCI. Imaging-guided PCI (with both OCT and IVUS) also resulted in improved stent expansion and acute stent-based procedural success compared to angiography-guided PCI.
Findings from the ILUMIEN III (OPTIMIZE PCI) trial were reported at the 28th annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium. Sponsored by the Cardiovascular Research Foundation (CRF), TCT is the world's premier educational meeting specializing in interventional cardiovascular medicine. The study was also published simultaneously in The Lancet.
Compared to angiographic-guidance, IVUS-guidance has been shown to reduce major adverse cardiovascular events (MACE) after PCI, mainly by resulting in a larger post-procedure lumen. Optical coherence tomography (OCT) provides higher resolution imaging than IVUS, although some studies have suggested it may lead to smaller luminal diameters after stent implantation.
The ILUMIEN III (OPTIMIZE PCI) study was a multicenter, prospective, randomized, controlled trial conducted at 29 sites in eight countries. Patients undergoing PCI were randomly assigned 1:1:1 to OCT-guidance, IVUS-guidance or angiography-guided stent implantation. OCT-guided PCI was performed using a specific protocol to determine stent length, diameter and expansion according to reference segment external elastic lamina (EEL) measurements. All patients underwent final OCT imaging (blinded in the IVUS and angiography arms).
Between May 2015 and April 2016, 450 patients were randomized and 415 final OCT acquisitions were analyzed for the primary endpoint of post-PCI MSA, measured by OCT at an independent core laboratory. The final MSA (median [25%, 75%]) was 5.79 [4.54, 7.34] mm2 with OCT-guidance, 5.89 [4.67, 7.80] mm2 with IVUS-guidance and 5.49 [4.39, 6.59] mm2 with angiography-guidance. The MSA with OCT-guidance was non-inferior to IVUS-guidance (one-sided 97.5% lower confidence interval = -0.70 mm2, Pnoninferiority=0.0014), but not superior (P=0.42).The trend toward greater MSA with OCT-
guidance compared to angiography-guidance did not reach statistical significance (P=0.12). Minimal and mean stent expansion and acute procedural success were greater in the imaging-guided arms compared to angiography.
Untreated major dissections were more common after IVUS-guided PCI than OCT-guided PCI (26.1% vs. 13.6%, P=0.0091). In the angiography-guided group, the rate of untreated major dissections was 18.6% (p=0.25). Similarly, compared with OCT-guidance, untreated major stent malapposition post-PCI was more frequent with both IVUS-guidance (20.7% vs. 10.7%, P=0.0221) and angiography-guidance (31.4% vs. 10.7%, p<0.0001). Clinical follow-up to one-year is ongoing in order to determine the clinical relevance of these OCT-based findings, as there were only six (1.3%) procedural and seven (1.6%) 30-day MACE events, with no significant differences between groups.
"The results of the ILUMIEN III (OPTIMIZE PCI) study show that using a specific reference segment EEL-based stent optimization strategy during OCT-guided PCI is safe and resulted in similar MSA compared to IVUS-guided PCI with fewer untreated major dissections and less major malapposition. OCT-guided PCI also led to greater stent expansion and procedural success compared to angiography-guided PCI," said lead investigator Ziad A. Ali, MD, DPhil. Dr. Ali is the Associate Director of Translational Medicine at the Center for Interventional Vascular Therapy at NewYork-Presbyterian Hospital/Columbia University Medical Center. He is also the Victoria and Esther Aboodi Cardiology Researcher and Louis V. Gerstner Scholar at Columbia University College of Physicians and Surgeons.
"These results are encouraging, but further study is still needed to determine whether the advantages we have identified by utilizing OCT-guidance will impact clinical outcome."
The ILUMIEN III (OPTIMIZE PCI) trial was funded by St. Jude Medical. Dr. Ali reported grants from St. Jude Medical, personal fees from St. Jude Medical, personal fees from ACIST Medical, and personal fees from Cardiovascular Systems Inc. outside the submitted work.
The CRF Clinical Trials Center conducted the site management, data management and monitoring, biostatistics and data analysis, and core lab analyses for the trial.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd