- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
IDSA releases guidelines for treatment of invasive aspergillosis
ARLINGTON, Va. – New therapies are improving care, but early diagnosis remains critical in the effective treatment of invasive aspergillosis, a potentially deadly fungal infection, according to new guidelines released by the Infectious Diseases Society of America (IDSA) and published in the journal Clinical Infectious Diseases.
The updated guidelines focus on the diagnosis and treatment of the major forms of aspergillosis: allergic, chronic and invasive, the latter which kills 40 percent to 80 percent of those with widespread infection.
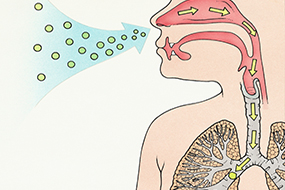
An airborne mold, aspergillus often is found in air conditioning units, compost piles and damp or flood-damaged homes or buildings. While generally harmless, it can cause an allergic reaction or chronic lung problems in some people and serious, invasive disease in vulnerable patients. Those at highest risk are people whose immune systems are suppressed, such as those undergoing stem cell and lung and other organ transplants. The infection also can affect those with severe influenza or who are on long-term steroids, or patients in the intensive care unit.
“Invasive aspergillosis often is overlooked, but early diagnosis and treatment are key,” said Thomas Patterson, MD, lead author of the guidelines and chief of the Division of Infectious Disease and professor of medicine at The University of Texas Health Science Center at San Antonio and South Texas Veterans Health Care System, San Antonio. “These are complicated infections with a number of treatment options. Patients really benefit from a multidisciplinary approach, including the expertise of an infectious disease specialist.”
Updating the 2008 guidelines, the new guidelines for the diagnosis and treatment of aspergillosis highlight the increased evidence for antifungal therapy recommendations as well as diagnostic tests.
The improved use of diagnostic tools has enhanced the ability to identify the infection early, the guidelines note. These include blood tests, cultures and computed tomography (CT) imaging. Because some of the methods are invasive – such as taking a culture directly from the lungs – physicians often are reluctant to proceed. Because the infection is so deadly, physicians should be aggressive in diagnosing patients suspected of having the infection, Dr. Patterson notes.
Additionally, new more-effective and better-tolerated antifungal medications, or versions of existing medications (e.g. extended release) have improved care, including isavuconazole and posaconazole. In some cases, combination therapy with voriconazole and an echinocandin is recommended for certain patients at highest risk.
Because invasive aspergillosis is so deadly, the guidelines recommend some patients at highest risk be treated with antifungals to prevent infection, including those with neutropenia and graft versus host disease (GVHD). Another prevention strategy is the use of special filtration systems for hospitalized immunosuppressed patients.
Invasive aspergillosis affects about 200,000 people worldwide, Dr. Patterson said. The allergic form is most common and affects more than 4 million people worldwide, according to the Centers for Disease Control and Prevention (CDC). Those with asthma and cystic fibrosis are at highest risk of developing allergic aspergillosis. The other major form is chronic pulmonary aspergillosis, which can affect healthy people, and occurs in about 400,000 people worldwide, the CDC notes. While requiring treatment, the allergic and chronic forms of aspergillosis typically aren’t deadly.
In addition to Dr. Patterson, the guidelines panel includes George R. Thompson III, David W. Denning, Jay A. Fishman, Susan Hadley, Raoul Herbrecht, Dimitrios P. Kontoyiannis, Kieren A. Marr, Vicki A. Morrison, M. Hong Nguyen, Brahm H. Segal, William J. Steinbach, David A. Stevens, Thomas J. Walsh, John R. Wingard, Jo-Anne H. Young and John E. Bennett.
IDSA has published more than 50 treatment guidelines on various conditions and infections, ranging from HIV/AIDS to Clostridium difficile. As with other IDSA guidelines, the aspergillosis guidelines will be available in a smartphone format and a pocket-sized quick-reference edition. The full guidelines are available free on the IDSA website at www.idsociety.org.
The updated guidelines focus on the diagnosis and treatment of the major forms of aspergillosis: allergic, chronic and invasive, the latter which kills 40 percent to 80 percent of those with widespread infection.
An airborne mold, aspergillus often is found in air conditioning units, compost piles and damp or flood-damaged homes or buildings. While generally harmless, it can cause an allergic reaction or chronic lung problems in some people and serious, invasive disease in vulnerable patients. Those at highest risk are people whose immune systems are suppressed, such as those undergoing stem cell and lung and other organ transplants. The infection also can affect those with severe influenza or who are on long-term steroids, or patients in the intensive care unit.
“Invasive aspergillosis often is overlooked, but early diagnosis and treatment are key,” said Thomas Patterson, MD, lead author of the guidelines and chief of the Division of Infectious Disease and professor of medicine at The University of Texas Health Science Center at San Antonio and South Texas Veterans Health Care System, San Antonio. “These are complicated infections with a number of treatment options. Patients really benefit from a multidisciplinary approach, including the expertise of an infectious disease specialist.”
Updating the 2008 guidelines, the new guidelines for the diagnosis and treatment of aspergillosis highlight the increased evidence for antifungal therapy recommendations as well as diagnostic tests.
The improved use of diagnostic tools has enhanced the ability to identify the infection early, the guidelines note. These include blood tests, cultures and computed tomography (CT) imaging. Because some of the methods are invasive – such as taking a culture directly from the lungs – physicians often are reluctant to proceed. Because the infection is so deadly, physicians should be aggressive in diagnosing patients suspected of having the infection, Dr. Patterson notes.
Additionally, new more-effective and better-tolerated antifungal medications, or versions of existing medications (e.g. extended release) have improved care, including isavuconazole and posaconazole. In some cases, combination therapy with voriconazole and an echinocandin is recommended for certain patients at highest risk.
Because invasive aspergillosis is so deadly, the guidelines recommend some patients at highest risk be treated with antifungals to prevent infection, including those with neutropenia and graft versus host disease (GVHD). Another prevention strategy is the use of special filtration systems for hospitalized immunosuppressed patients.
Invasive aspergillosis affects about 200,000 people worldwide, Dr. Patterson said. The allergic form is most common and affects more than 4 million people worldwide, according to the Centers for Disease Control and Prevention (CDC). Those with asthma and cystic fibrosis are at highest risk of developing allergic aspergillosis. The other major form is chronic pulmonary aspergillosis, which can affect healthy people, and occurs in about 400,000 people worldwide, the CDC notes. While requiring treatment, the allergic and chronic forms of aspergillosis typically aren’t deadly.
In addition to Dr. Patterson, the guidelines panel includes George R. Thompson III, David W. Denning, Jay A. Fishman, Susan Hadley, Raoul Herbrecht, Dimitrios P. Kontoyiannis, Kieren A. Marr, Vicki A. Morrison, M. Hong Nguyen, Brahm H. Segal, William J. Steinbach, David A. Stevens, Thomas J. Walsh, John R. Wingard, Jo-Anne H. Young and John E. Bennett.
IDSA has published more than 50 treatment guidelines on various conditions and infections, ranging from HIV/AIDS to Clostridium difficile. As with other IDSA guidelines, the aspergillosis guidelines will be available in a smartphone format and a pocket-sized quick-reference edition. The full guidelines are available free on the IDSA website at www.idsociety.org.
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd