- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Hysteroscopic sterilization or Surgical sterilization: JAMA study
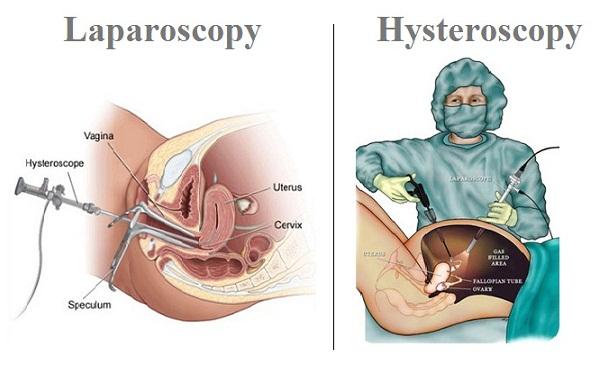
Bottom Line: Hysteroscopic sterilization, a non-surgical procedure that involves placing small implants in the fallopian tubes to render a woman infertile, was associated with an increased risk of gynecological complications (most notably sterilization failure with subsequent pregnancy) compared to surgical sterilization, but there were no differences between the two approaches in medical outcomes.
Why The Research Is Interesting: In developed countries, two main types of female sterilization are available: hysteroscopic and laparoscopic, the latter involving general anesthesia and a small incision in the abdominal wall. Safety concerns related to hysteroscopic sterilization were raised in the United States in 2015 by women who reported to the U.S. Food and Drug Administration (FDA) large numbers of adverse events, including bleeding, unwanted pregnancy, abdominal pain, depression, and thyroid disorders.
Who and When: 105,357 women in France who underwent hysteroscopic sterilization (n = 71,303) or laparoscopic sterilization (n = 34,054) between 2010 and 2014 and followed up through December 2015.
What (Study Measures): Risks of procedural complications (surgical and medical), gynecological complications (sterilization failure that includes second sterilization procedure or pregnancy) and medical outcomes (including all types of allergy; autoimmune diseases; thyroid disorder; use of analgesics, antimigraines, antidepressants, outpatient visits; sickness absence; suicide attempts; death) that occurred within one and three years after sterilization.
How (Study Design): This is an observational study. Because researchers are not intervening for purposes of the study they cannot control natural differences that could explain the study findings.
Authors: Mahmoud Zureik, M.D., Ph.D., French National Agency for Medicines and Health Products Safety, Saint-Denis, France and coauthors
Results: Compared with laparoscopic sterilization, hysteroscopic sterilization was:
-- Associated with a lower immediate risk of procedural complications
-- Associated with a higher risk of gynecological complications
-- Not associated with an increased risk of certain medical outcomes
Study Limitations: Administrative databases were used to investigate a possible role of hysteroscopic sterilization in notified complaints. All individual disorders reported by patients or physicians and collected into medical device vigilance databases could not be examined.
To read the article click on the link below.
http://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2017.21269

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd