- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
How to treat PPI-refractory GERD
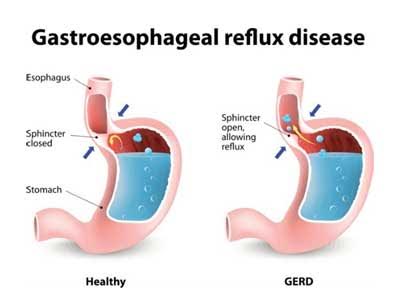
Gastroesophageal reflux disease (GERD) is a digestive disorder that affects lower esophageal sphincter (LES), the muscle ring between stomach and esophagus. It occurs when bile or stomach acid flows into the food pipe and irritates the food-pipe lining.
Proton pump inhibitors (PPIs) are a type of medication that can be used for reduction of stomach acid and relieve the symptoms of GERD. However, a significant percentage of patients with GERD do not respond to PPI therapy. The causes for PPI-refractory GERD include adherence, persistent acid, functional disorders, nonacid reflux, and PPI bioavailability.
Rena Yadlapati, Anschutz Medical Campus, University of Colorado, Aurora, CO, USA, and colleagues conducted a study to assess expert gastroenterologists opinion on treatment for distinct GERD profiles characterized by PPI unresponsive symptoms. The study was published in The American Journal of Gastroenterology.
For the study, fourteen esophagologists applied the RAND/UCLA Appropriateness Method to hypothetical scenarios with previously demonstrated GERD (positive pH-metry or endoscopy) and persistent symptoms despite double-dose PPI therapy undergoing pH-impedance monitoring on therapy. A priori thresholds included: esophageal acid exposure (EAE) time >6.0%; symptom-reflux association: symptom index >50% and symptom association probability >95%; >80 reflux events; large hiatal hernia: >3 cm.
Primary outcomes were the appropriateness of four invasive procedures (laparoscopic fundoplication, magnetic sphincter augmentation, transoral incisionless fundoplication, radiofrequency energy delivery) and preference for pharmacologic/behavioral therapy.
Key findings of the study include
- Laparoscopic fundoplication was deemed appropriate for elevated EAE, and moderately appropriate for a positive symptom-reflux association for regurgitation and a large hiatal hernia with normal EAE
- Magnetic sphincter augmentation was deemed moderately appropriate for elevated EAE without a large hiatal hernia
- Transoral incisionless fundoplication and radiofrequency energy delivery were not judged appropriate in any scenario
- Preference for non-invasive options was as follows: H2RA for elevated EAE, transient lower esophageal sphincter relaxation inhibitors for elevated reflux episodes, and neuromodulation/behavioral therapy for positive symptom-reflux association
Recommendation
For treatment of PPI unresponsive symptoms in proven GERD, expert esophagologists recommend invasive therapy only in the presence of abnormal reflux burden, with or without a hiatal hernia, or regurgitation with a positive symptom-reflux association and a large hiatus hernia. Non-invasive pharmacologic or behavioral therapies are preferred for all other scenarios.
For further information click on the link: 10.1038/s41395-018-0045-4

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd