- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
How Helicobacter pylori causes gastric cancer
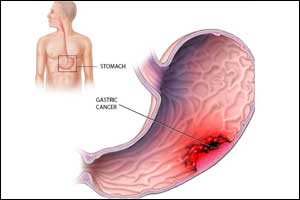
Gastric cancer is one of the five most fatal types of cancer. According to the statistics of the World Health Organization (WHO), about 750,000 patients die each year after developing the disease. The main cause is thought to be the bacterium Helicobacter pylori (H. pylori). At present, there are no effective therapies for gastric cancer and growing spread of antibiotic resistance is further complicating treatment of the infection. Researchers at Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) have now identified two mechanisms through which this bacterium can cause gastric cancer. Their findings could result in the development of new therapeutic approaches.
The international team of scientists headed by Dr. Nicole Tegtmeyer of the Chair of Microbiology at Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) investigated how bacteria destroy the stomach's protective layer. This protective layer is composed of densely packed epithelial cells that protect the stomach against the effects of gastric acid. The researchers have now discovered that H. pylori secretes an enzyme, a protease called HtrA, which it uses much like a weapon to penetrate this protective layer. HtrA cleaves the three proteins occludin, claudin-8 and E-cadherin, rupturing the layer of epithelial cells. As a result, the H. pylori bacteria can access deeper, normally pathogen-free tissue layers, and inflict further damage. This is the first step towards gastric cancer starting to develop.
This first phase, however, is followed by one that is even more dangerous, as the team discovered. Needle-like protrusions, termed type IV secretion systems, are activated and function as 'molecular syringes'. Using a receptor-dependent mechanism, these inject a bacterial toxin, the CagA protein, through the basolateral membrane of the host cells. The injected CagA subsequently reprograms host cells, making them potentially cancerous. Another effect of this protein is that it prevents the human immune system from recognizing and eliminating the bacteria - a crucial mechanism for the long-term survival of H. pylori in the human stomach.
A new approach to treating gastric cancer
Dr. Tegtmeyer expects these findings will make it possible to develop important new antibacterial therapeutic approaches, as HtrA and CagA are ideal novel drug targets. The team has already started to test specific HtrA inhibitors. "We hope that suitable active agents can either completely prevent infection or inhibit the injection of CagA," explains Tegtmeyer.
For more details click on the link: http://dx.doi.org/10.1016/j.chom.2017.09.005

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd