- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Hirsutism - Standard Treatment Guidelines
Hirsutism is the presence of excessive growth of terminal hair that appears in a male pattern in a woman. Though the presence of hirsutism may be a purely cosmetic and social concern to the affected woman, medically it can be indicative of conditions like Polycystic Ovarian Syndrome (PCOS), non classic Congenital Adrenal Hyperplasia (CAH) or virilizing tumours of the ovaries or adrenals.
Androgens are essential for the conversion of vellus (small, straight and fair) hairs into terminal (larger,thicker,coarser, curlier and darker) hairs. This conversion is dependent on the level of the circulating androgens, their metabolism locally at the pilo-sebaceous unit by the enzyme 5 alpha reductase into dihydrotestosterone, and the subsequent binding of the latter to its receptor. This local metabolism and androgen-receptor interaction is highly variable. As a result pilosebaceous units vary in their sensitivity to androgen. Therefore, the degree of hirsutism may be very different between individuals with similar levels of circulating androgens.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Hirsutism. Following are the major recommendations :
Case definition:
Hirsutism is a clinical diagnosis. Hirsutism should be distinguished from hypertrichosis which is generalised excessive vellus hair growth in a non sexual pattern. Hypertrichosis is androgenindependent. Its origin is hereditary or secondary to systemic conditions and certain drugs.
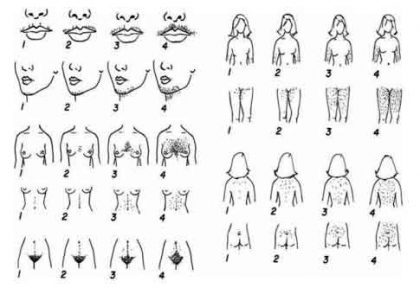
Typically, hirsutism is defined clinically by judging the severity of hirsutism (graded subjectively from 1 to 4) in each of nine defined body areas. A total score of more than 8 out of a maximum of 36 is considered significant. This is the Ferriman-Gallwey hirsutism scoring system. Apart from its subjective nature and other drawbacks, the total score does not reflect the significance of higher degrees of hirsutism in one area alone ("focal hirsutism") if the other areas are unaffected. Thus focal hirsutism which is causing distress to a woman may not lead to a "significant" total FG score of 8. This has led to the concept of "patient-important hirsutism" – i.e. hirsutism that is significant for the individual seeking medical attention.
Incidence of The Condition In Our Country :
About 5 % of women in the west have hirsutism. Data for our country are lacking. It is encountered commonly in practice.
ETIOLOGY:
Polycystic ovary syndrome
Idiopathic (hirsutism without hyperandrogenemia)
Late-onset or non-classic congenital adrenal hyperplasia
Androgen-secreting tumours
Ovarian tumours
Adrenal tumours
Cushing's syndrome
Hyperprolactinaemia
Acromegaly
Thyroid dysfunction
Iatrogenic
Androgen therapy (testosterone, anabolic steroids)
Danazol
Androgenic progestins (levonorgestrel, norethindrone and norgestrel)
Glucocorticoids
Polycystic ovaries, idiopathic hirsutism and drug-induced hirsutism constitute the largest proportion of cases.
Hypertrichosis can occur in the following conditions or with some drugs as indicated below
Porphyria
Phenytoin
Cyclosporine
Counselling
Patients have to be informed of treatment options and time frame of efficacy of various modalities – especially the delayed onset of pharmacologic therapy and that laser and intense pulsed light (IPL) modalities are methods of long term hair reduction and not "permanent" removal. The need for continued therapy for sustained control should also be explained.
Optimal Diagnostic Criteria, Investigations, Treatment And Referral Criteria :
Diagnosis:
Hirsutism is a clinical diagnosis. The presence of excess terminal hairs in a male pattern has to be documented. The Ferriman Gallewey score of > 8 is helpful if the scoring is feasible. A baseline FG score is also useful for assessing treatment response.
Strict requirement of FG score >8 for diagnosing and treating hirsutism is not applicable. Some patients have already removed their hair or have been treated before their first medical encounter precluding any scoring attempt. One also has to bear in mind the situation of "focal hirsutism" and "patient-important hirsutism".
The Ferriman Gallwey Scoring System
Hirsutism is scored from 0 (none) to 4 (severe) in each of nine defined areas, and the total score added.
Clinical evaluation is also directed at discerning clues to specific etiologies.
- Drug use
- Androgen secreting neoplasm: Sudden onset, rapid course, progression, virilisation (clitoromegaly, temporal hair recession, muscularity, voice change) or abdominal/pelvic mass suggest the possibility of androgen secreting neoplasm.
- PCOS : Perimenarcheal onset of menstrual irregularity, infertility, acne, male-pattern alopecia, obesity, acanthosis nigricans.
- Non-classic CAH: history of consanguinity in parents, family history of infertility, hirsutism, menstrual irregularity or both
- Cushing's syndrome: Hypertension, striae, easy bruising
- Hyperprolactinemia: Galactorrhoea
- Primary hypothyroidism: Goitre, other clinical features
- Acromegaly: Acral enlargement, coarse features, prognathism
Investigations:
Patients with isolated, mild hirsutism need not have any tests done.
Patients with the following need to be investigated:
Moderate or severe hirsutism, i.e. FG score >15
Hirsutism of any degree when it is
sudden in onset and/or rapidly
progressive progressing despite therapy
associated with menstrual irregularity/infertility/obesity/acanthosis nigricans
associated with features of virilization
1. Serum Testosterone:
Serum testosterone should be checked early morning. In women who are having regular cycles it should be checked between days 4-10. In others, either a random sample or one obtained after progesterone induced bleeding should be used. Testosterone levels in the upper normal range or mildly elevated (70 -150 ng/dl) is usual for PCOS. Serum testosterone values in the adult normal male ranges (200 – 1100 ng /dl) are seen in virilizing neoplasms. If serum total testosterone is normal in the situation where elevated levels are expected, serum albumin and SHBG should be checked in addition and the free androgen index calculated. Commercially available free testosterone assays may be unreliable.
2. Other tests are to be chosen according to the suspected etiology
- Ultrasound : PCOS, adrenal/ovarian neoplasm
- Serum basal 17 hydroxy progesterone and if this is between 3 -10 ng/ml a Synacthen stimulation test : non classic CAH
- Serum DHEAS : Adrenal neoplasm
- Additional tests for hypothyroidism, hyperprolactinemia, acromegaly, Cushing 's syndrome, when suspected
Treatment :
Treatment has to be prolonged and often continuous for control of hirsutism. When cosmetic measures alone are insufficient treatment, it has to be complemented with (a) pharmacologic therapy, or (b) direct long term hair removal methods. The choice between pharmacological therapy and hair removal methods depends on patient preference, cost, and the area needed to be treated (wider areas require pharmacologic therapy). In those with hyperandrogenemia, pharmacologic therapy needs to be combined with hair removal methods to achieve better control of hirsutism.
1. Pharmacologic therapy :
Any chosen pharmacologic therapy needs to be given a trial of at least six month before augmenting dosage, combining, or changing drugs.
- Oral contraceptives : OCPs containing progestin with less (norgestimate, desogestrel) or no (drospirenone) androgenic potential are better than those containing levonorgestrel.
- Antiandrogens : Because of their teratogenic potential, antiandrogens should not be used alone in all those who can conceive and are not on effective contraception.
Spironolactone is the most commonly used antiandrogen at 100-200 mg/day in divided doses. Finasteride at 2.5 to 5 mg per day is less effective. It is a type 2 alpha reductase inhibitor and inhibits conversion of only one of the isoenzymes responsible for formation of dihydrotestosterone from testosterone.
Flutamide (250-500 mg per day) is rarely used because of its hepatotoxic potential but can be used with periodic monitoring of LFT in severe refractory cases.
Topical eflornithine cream is used for focal hirsutism (e.g. facial hirsutism). It inhibits ornitihine decarboxylase which catalyses the rate limiting step for polyamine synthesis which is necessary for hair growth. It does not remove hair but reduces the growth and appearance of facial hair.
2. Hair removal/reduction methods :
- Temporary
Depilation - Removal of hair shaft from the skin surface e.g. shaving and chemical depilatory creams
Epilation – Removal of hair shaft from above the bulb – waxing and plucking
- "Permanent" methods of hair reduction
Electrolysis – destruction of hair follicles by insertion of a needle and use of electric current can be used for limited focal hairs as it is time consuming. The cost is less than photoepilation.
Photoepilation (laser or intense pulsed light) is a costly modality, but can be used for treating relatively wider areas.The energy absorbed by the melanin destroys the hair follicles. There is a reduction of 30 % or more in the number of terminal hair after a given setting. More than one sitting is therefore required. Vellus hair follicles remain and can exhibit conversion into terminal hairs when androgen excess is not taken care of.
Standard Operating Procedure :
- Confirm hirsutism. Distinguish from hypertrichosis.
- Ascertain history of development and progression of hirsutism.
- Check for other features of hyperandrogenism (acne, male-pattern alopecia), virilisation
- Rule out exposure to androgens, and features of PCOS, Cushing's syndrome, acromegaly, hyperprolactinemia and hypothryoidism.
- Isolated mild hirsutism in women with normal cyclical menstruation, does not require further testing unless there is inadequate response to or progression despite empirical treatment.
- Total testosterone should be checked in all others. Free testosterone index in case the latter is unexpectedly normal.
- Other tests would depend on the endocrinopathy clinically suspected.
- Treatment is offered to all women with patient-important hirsutism despite cosmetic measures.
- Pharmacotherapy and electrolysis/photoepilation are the available options – choice for latter measures being made on patient preference, availability, affordability and extent of area affected. Pharmacotherapy often needs to be combined with hair reduction methods in women with hyperandrogenemia to achieve better and sustained control.
- Pharmacotherapy is precluded in all those trying to or likely to conceive
- OCPs alone are an option for most. Antiandrogens alone can be used only in those who follow effective contraception. Antiandrogens and OCPs are therefore often used in combination.
- Any pharmacotherapy should be given a trial of at least 6-9 months before modification.
Referral criteria
- When endocrinological conditions like acromegaly, Cushing's syndrome, CAH are suspected
- When facilities for photoepilation or electrolysis is not available.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd