- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Haemorrhoids - Standard Treatment Guidelines
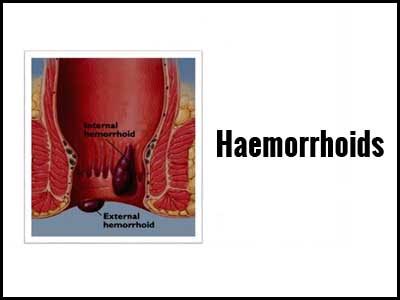
Three haemorrhoidal cushions are found in the left lateral, right anterior and right posterior positions of the anal canal. Bleeding results when these cushions are engorged and subjected to raised intra abdominal pressure while straining during defecation.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Haemorrhoids. Following are the major recommendations :
Definition :
Haemorrhoids are cushions of submucosal tissue containing venules, arterioles and smooth muscle fibers located in the anal canal.
Treatment is indicated only if they become symptomatic due to venous engorgement of the haemorrhoidal plexus.
Incidence :
Haemorrhoids is a common condition but the exact incidence in our country is not documented.
Differential Diagnosis
- Prolapsed rectum
- Anal fissure
- Anal polyp
- Carcinoma anal canal
- Rectal varices due to portal hypertension
- Perianal abscess
- Proctitis
Prevention & Counselling
Excessive straining, increased intra abdominal pressure and hard stools increase venous engorgement of haemorrhoidal plexus. Avoidance of these would prevent the development of haemorrhoids.
Optimal Diagnostic Criteria :
Situation 1: Diagnosis is largely
Clinical Diagnosis
Symptoms:
- Bleeding per rectum, bright red, painless
- Anemia due to frequent bleeding
- Mass prolapsing per rectum
- Pain on prolapsed
- Mucous discharge
- Pruritus
- Skin tag
Examination
Direct Visulisation : thrombosed/prolapsed haemorrhoids, external haemorrhoids & skin tags be visualized.
Digital Rectal Examination :
Thrombosed haemorrhoids, as well as other associated conditions such as anal cancer, BPH may be felt per rectum.
Proctoscopy :
Internal haemorrhoids occur in 3, 7 & 11 “o” clock positions. These are visualized during prctoscopy. Haemorrhoids are classified into 4 graes by descent
Grade Presentation
- Bleeding
- Protrusion below the anal verge while straining with spontaneous reduction
- Protrusion regressing with manual reduction
- Irreducible protrusions
Based on their location, haemorrhoids can be classified into
External – located distal to dentate line, covered by anoderm, painful, arise from inferior haemorrhoidal plexus
Internal – located prominal to dentate line, covered by insensuate anorectal mucosa, painless, may prolapsed or bleed
Interno – external – features of both
Investigations:
Hb
Peripheral smear
TLC, DLC, ESR
Blood grouping and Rh typing
USG abdomen
Treatment:
Medical :
- Laxatives
- Haematinics if anemia is present
- Sitz bath
- Ointment
- Antibiotics when infection or complications are present
- Emergency transfusion when presentation is of profuse haemorrage or severe anaemia due to chronic blood loss
Surgical :
I. Minor Outpatient procedures:
1. Sclerotherapy – for grade 1 & II haemorrhoids and bleeding haemorrhoids
2 to 5 ml of 5% phenol in almond oil injected around pedicle in the submucosa aseptically
2. Banding – gr II & III haemorrhoids by modified Barron’s band applicator above the dentate line
In patient
GR III & IV haemorrhoids
1. Haemorrhoidectomy
- Open: MILLIGAN – MORGAN operation
- Closed: HILL – FERGUSON operation
2. Excision of thrombosed pile mass:
ANESTHESIA: GA/Spinal/Caudal block
Referral criteria:
Patients who opt for stapled haemorrhoidopexy
Patients with portal hypertension
Patients with bleeding disorders
Patients with co-morbidities that may require ICU care
SOP
Outpatient / day care procedures: Minor procedures for Grade I & II
In Patient: Operative procedures for Grade III & IV
Situation 2:
Clinical Diagnosis
Symptoms:
- Bleeding per rectum, bright red, painless
- Anemia due to frequent bleeding
- Mass prolapsing per rectum
- Pain on prolapsed
- Mucous discharge
- Pruritus
- Skin tag
Examination
Direct Visulisation : thrombosed/prolapsed haemorrhoids, external haemorrhoids & skin tags be visualized.
Digital Rectal Examination :
Thrombosed haemorrhoids, as well as other associated conditions such as anal cancer, BPH may be felt per rectum.
Proctoscopy :
Internal haemorrhoids occur in 3, 7 & 11 “o” clock positions. These are visualized during proctoscopy. Haemorrhoids are classified into 4 grades by descent.
Grade Presentation
- Bleeding
- Protrusion below the anal verge while straining with spontaneous reduction
- Protrusion regressing with manual reduction
- Irreducible protrusions
Based on their location, haemorrhoids can be classified into
External – located distal to dentate line, covered by anoderm, painful, arise from inferior haemorrhoidal plexus
Internal – located prominal to dentate line, covered by insensuate anorectal mucosa, painless, may prolapsed or bleed
Interno – external – features of both
Investigations:
Hb
Peripheral smear
TLC, DLC, ESR
Blood grouping and Rh typing
USG abdomen
Colonoscopy – to r/o other conditions (malignancy) and co-existing when required
Coagulation profile
Treatment:
Medical :
- Laxatives
- Haematinics if anemia is present
- Sitz bath
- Ointment
- Antibiotics when infection or complications are present
- Emergency transfusion when presentation is of profuse haemorrage or severe anaemia due to chronic blood loss
Surgical :
I. Minor Outpatient procedures:
1. Sclerotherapy – for grade 1 & II haemorrhoids and bleeding haemorrhoids
2 to 5 ml of 5% phenol in almond oil injected around pedicle in the submucosa aseptically
2. Banding – gr II & III haemorrhoids by modified Barron’s band applicator above the dentate line
In patient
GR III & IV haemorrhoids
1. Haemorrhoidectomy
- Open: MILLIGAN – MORGAN operation
- Closed: HILL – FERGUSON operation
2. Excision of thrombosed pile mass:
ANESTHESIA: GA/Spinal/Caudal block
Outpatient procedures:
1. Photocoagulation – 1&II degree haemorrhoids
Infrared coagulation probe applied to the apex of each haemorrhoid to coagulate the underlying venous plexus
In-patient procedures:
1. Stapled haemorrhoidectomy: for grade III haemorrhoids. May be done as a day care procedure or as an in-patient
SOP:
In-patient
Day care procedure – depending on the education and awareness of the patient
WHO DOES WHAT?
Doctor
- Clinical examination
- Diagnosis
- Planning surgery
- Surgery
- Post op care
- Anesthesia
Nurse
- Pre & post operative care
- Assisting during surgery
Technician
- Pre operatively equipment and drugs to be checked and kept ready
- Assist anesthetist in the OT
- Assist the surgeon, positioning of the patient
Resources Required For One Patient / Procedure (Patient weight 60 Kgs)
| Situation | Human Resources | Investigations | Drugs/Consumables | Equipment |
| 1. | Surgeon – 1 Medical Officer / Assistant Surgeon - 1 Staff Nurse – 1 Technician – 1 Nursing Orderly – 1 Sweeper - 1 | Haemogram Urine Analysis Blood Sugar | Antibiotics Analgesics IV fluids Sutures Anesthetic drugs lignocaine | OT Table & lights Autoclave General surgery set Cautery Suction Anesthesia equipment |
| 2. | Consultant – 1 Resident – 1 Staff nurse – 1 Technician – 1 Nursing orderly -1 Sweeper - 1 | Same as above + HbA1C Coagulation Profile ECG X-Ray chest | Same as above | Same as above |
Guidelines by The Ministry of Health and Family Welfare :
Dr Ajit Sinha Department of Surgery Safdarjung Hospital New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd