- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Haematuria-Standard Treatment Guidelines
Hematuria is the presence of red-blood cells (RBC) in urine.
- It may be categorized as gross (visible to naked eye) or microscopic (detected in urine microscopy). The recommended definition of microscopic hematuria is three or more red blood cells per high-power field on microscopic evaluation of urinary sediment from two of three properly collected urinalysis specimens.
- It may arise from any part of the urinary tract, from glomerulus to meatal tip and may be characterized as initial, terminal or total, which points to the approximate site of origin (distal to external sphincter, proximal urethra-bladder neck, and bladder and upper tracts, respectively).
- Severity of hematuria bears no relation with the etiology, therefore, its presence must be considered serious unless proven otherwise.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Haematuria.
Following are the major recommendations :
Prevalence
The prevalence of asymptomatic microscopic hematuria varies from 0.19 percent to as high as 21 percent any varies widely with different age groups.
Differential diagnosis
Hematuria is a manifestation of a myriad of varied clinical diagnoses ranging from exercise-induced to cancer-related. The differential diagnosis can be classified on the basis of site of origin as shown below:
| Origin | Etiologies |
| Glomerular | Acute glomerulonephritis, lupus nephritis, benign familial hematuria, Berger's disease, Goodpasture's disease, exercise hematuria. |
| Renal | Polycystic kidney disease, Medullary sponge kidney, papillary necrosis, renal infarct, lymphoma, multiplemyeloma, amyloidosis, inflammation and infections, vascular malformation |
| Urologic | Neoplasia, calculi, benign Prostatic hyperplasia, urethral stricture, endometriosis, diverticulitis, infection, foreign body, GUTB |
| Adjacent organ | Abdominal aortic aneurysm, appendicitis, infiltrating malignancy |
| Hematologic | Congenital and acquired coagulopathy, therapeutic anticoagulation, sickle-cell disease and trait, sickle-cell thalassaemia, sickle-cell Hemoglobin-C disease |
| Fictitious | Vaginal bleed |
| False hematuria | Food pigments, drug metabolites, malingering |
Diagnosis and evaluation
Once a patient presents with history of hematuria, first step is detailed history and clinical examination.
1.History should include nature of hematuria whether intermittent / continuous, total / initial / terminal, or episodic.
2. Associated symptoms
3. passage of stones, tissues, clots; shape of clots (tubular, small).
4. Lower urinary tract symptoms (poor stream, frequency, urgency, nocturia, incontinence, dysuria, etc.
5. Pain, location (flank, groin, suprapubic, other), nature and other characteristics.
6. History of fever, facial puffiness, pedal edema.
7. Medications (e.g. oral contraceptives, analgesics, anticoagulants, others)
8. Co-morbidity like tuberculosis, diabetes mellitus, hypertension,
9. Coagulation disorders and family history of renal disease.
10. General physical examination and a focused examination pertaining to genitourinary system.
Next step is to perform a urine microscopy to confirm presence of RBCs and to rule out other causes of red brown colour in urine;
Dipstick tests commonly available will be positive in presence of RBCs, hemoglobin or myoglobin, therefore not specific for hematuria. Therefore, a positive dipstick must be followed by a microscopy.
Urine analysis
- Ideally the sample is collected in the lab. rather than brought from home (a urine sample not freshly voided or collected from drainage bag is unreliable for analysis).
- For male and female adults, clean catch mid-stream urine sample should be evaluated. In female the technique is similar but requires more attention as chances of contamination are much higher.
- In children the method is similar for those who can be made to follow the instructions. Otherwise, after cleansing, a sterile plastic bag is placed over penis / vulva. In case the specimen is not satisfactory, suprapubic aspiration may be done (easy in small children because intra-abdominal location of bladder).
One aliquot of the sample is subjected to routine examination (color, transparency, specific gravity, chemical analysis for pH, protein, etc.).
Ten milliliters of the second aliquot of urine is centrifuged at 2000rpm for 5min, and supernatant is discarded.
The sediment is re-suspended, a drop of which is examined under microscope for cells, crystals and casts.
RBCs are easily visible in X400 power. Microhematuria is diagnosed in presence of more than 3 RBCs per high power field in adults and 5 or more in children and in trauma cases. The morphology of RBC as well as presence of RBC clumps and casts should be seen. Phase contrast microscopy is the best way to detect dysmorphic RBCs. Dysmorphic RBCs are suggestive of a renal or glomerular source of hematuria.
Hematuria must be interpreted as part of complete urine analysis, as presence of other anomalies e.g. proteins, casts, crystals and pus cells, etc. may suggest towards diagnosis.
After confirmation of erythrocytouria, the next logical step is to differentiate between:
- Glomerular hematuria (presence of dysmorphic RBC, and RBC casts and clumps and usually associated with proteinuria).
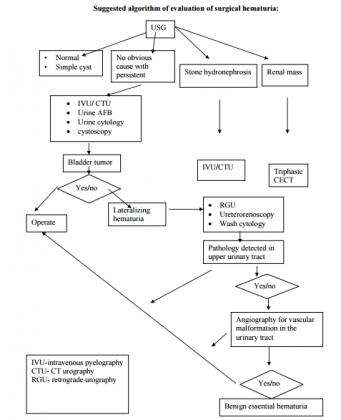
- Nonglomerular hematuria - an ultrasonography of abdomen is the next step to detect any anatomical abnormality in the urinary tract (e.g. stones, renal cysts, renal mass, bladder tumor, prostatomegaly, hydronephrosis, etc.).
- For those with history suggestive of infection and associated pyuria, a urine culture and sensitivity should be done to rule out infection,
- Complete blood count, renal functions, blood sugar and coagulogram (if appropriate), must be done to rule out other causes and as a part of workup for surgery if an abnormality is detected on ultrasonography.
In absence of features of glomerular hematuria, urinary tract infection and USG evidence of renal mass, most patients would require cystourethroscopy. Certain investigations are suggested, before proceeding for the same-
- Urine cytology for malignancy
- Urine for AFB
- Intravenous urography / CT urography.
Management:
After complete evaluation approximately overall, 1/3rd will have origin in kidney and the rest in middle and lower urinary tract.
- Further management needed in,
- 25% with urinary tract infection
- 20% will be diagnosed as malignancy (bladder cancer, kidney cancer),
- 20% with urinary stone disease.
- Rest 15% other causes
- 20% are diagnosed as benign essential hematuria (of obscure origin) and these require careful follow up.
Treatment is guided by the underlying cause of hematuria.
As general practitioners are the frequently the first contact clinicians, they should perform the initial workup (urine analysis, urine culture, ultrasonography) and based on the presentation and these investigation. Uncomplicated UTIs may be managed at the community level. Others should be referred to appropriate specialist (nephrologists, urologist).
Those with glomerular cause of hematuria (fever , facial puffiness, pedal edema, hypertension and presence of dysmorphic RBCs on microscopy) require a nephrology referral for further diagnosis and management.
Those patients diagnosed with a malignancy/renal stone as the cause, need appropriate urology referral to a higher center for further evaluation and management.
Resources required
1.Facility for routine and microscopy of the urine.
2.Ultrasonography.
3.Microbiological services.
4.Radiological services (preferably with facility of computed tomography).
Guidelines by The Ministry of Health and Family Welfare :
Prof. Rajesh Ahlawat
Chairman,
Department of Urology & Kidney Transplant,
Medanta Medicity
Reviewed By:
Dr Anup Kumar Gupta
Head of Department
Department of Urology
VMMC and Safdarjang Hospital,
New Delhi
bladder cancerCT urographyDr Anup Kumar GuptaguidelinesHaematuriaHematologickidney cancerMicrohematuriaProf Rajesh AhlawatRBCtreatment guidelinesUltrasonographyUrologic
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd