- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
GOI Antibiotic Guideline For Pediatric Infections

In 2016, National Centre For Disease Control, Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India came out with National Treatment Guidelines for Antimicrobial Use in Infectious Diseases. Following are its major recommendations:-
Specific Conditions
For Infant below 2 months age (more than 2kg):
For 2 months and above-
Inj Ceftriaxone (100mg/kg/day-2 divided dosage) for 10 -14 days
2nd line therapy: Meropenem (120 mg/kg/day in 3 div doses) + Vancomycin (60mg /kg/day in 4 div doses) for 10-14 days
Chemoprophylaxis for Meningococcal Disease Contacts (including non-vaccinated Hospital Staff): To be effective in preventing secondary cases, chemoprophylaxis must be initiated as soon as possible (i.e. not later than 48 hours after diagnosis of the case). Mass chemoprophylaxis not needed.
LOWER RESPIRATORY TRACT INFECTION-
Community acquired Pneumonia is categorized in to 2 types –Severe pneumonia (those with respiratory distress) and pneumonia (those with fast breathing only, treated on OPD basis).
For Severe Pneumonia (Children with respiratory distress requiring indoor care)-
Whenever Staphyloccus aureus is suspected in children (see Text Box), the various drug options are:
For pneumonia (OPD)
Routine use of macrolide antibiotics for all cases of pneumonia is not advocated. Recent data suggests that (i) the routine addition of macrolides to children with CAP does not improve outcome (ii) selective use of macrolides would reduce their indiscriminate use and reduce antibiotic resistance.
Classically the mycoplasma pneumonia presents in an atypical fashion but literature suggests that it can sometimes be difficult to distinguish mycoplasma pneumonia from a pyogenic pneumonia.
Macrolide antibiotics should be considered in following clinical scenarios where the likelihood of mycoplasma pneumonia is high:
In the first two conditions macrolide antibiotics can be used along with the first line therapy for CAP.
EMPYEMA
Antimicrobial Therapy:
VENTILATOR ASSOCIATED PNEUMONIA:
Treat as per the sensitivity pattern of your ICU.
General Suggestion:
Second line Therapy
Third line Therapy
UPPER RESPIRATORY TRACT INFECTIONS
As these are mostly viral in origin, antibiotics are not needed barring following situations
Bacterial Pharyngotonsillitis (Group A Streptococcus)-
While Penicillin is the drug of choice Amoxycillin is good alternative and used widely.
If the patient is Pencillin allergic, the alternative drugs are
Faucial diphtheria
Acute otitis media (AOM)-
Mastoiditis And Other Acute Ear Infection
CSOM
Acute Sinusitis with URI-
Ludwig’s Angina
Pertussis
GASTRO-INTESTINAL DISEASES
Dysentery
(a) For inpatients- Inj Ceftriaxone (100mg/kg) for 5-7 days.
(b) For OPD cases
Cholera
Enteric Fever
(a) For OPD cases-
(b) For inpatients
a) Ofloxacin 15mg/kg/d in two divided doses for 10-14 days. Antibiotic therapy should be continued till one week post-fever defervescence.
b) Chloramphenicol (50- 75mg/kg/day PO) x 14 days.
c) TMP-SMX (8 mg/kg/day of TMP PO) x 14 days.
Peritonitis
For primary peritonitis in nephrotic syndrome: Inj. Ampicillin + Aminoglycoside OR inj. cefotaxime for primary peritonitis in a cirrhotic, inj. cefotaxime.
Liver Abscess
Total duration of therapy is 4-6 weeks
URINARY TRACT INFECTION (UTI)
a) Uncomplicated UTI (age> 2 months with lower UTI, without any urinary tract obstruction) -
Oral Cotrimoxazole (8-10mg of TMP component) /kg/day oral BD
OR
Cefixime (8-10 mg/kg/day BD) to be given for 7-10 days
OR
Co Amoxycillin+Clavulanic Acid (30-50 mg of Amoxicillin) for 7-10 days.
b) Complicated / Severe UTI (Febrile UTI, Systemic toxicity, renal angle tenderness or with any urinary structural abnormality) and all UTI in children less than 2 months should be treated with parenteral antibiotics.
Inj. Cefotaxime (150-200mg/kg/day 8h OR
Inj. Ceftriaxone (100mg/kg/day OD OR
Inj. Amikacin 15mg/kg OD
To be given for 10-14 days
c) In Immunocompromised host/ severe systemic sepsis or as second line for complicated UTI-
Inj. Piperacillin Tazobactum 90mg/kg/dose IV 6h) or Inj. Meropenem (20-40mg/kg/dose 8h) To be given for 10-14 days
FEBRILE NEUTROPENIA
Presumptive therapy for initial antimicrobial coverage in critically ill children with severe sepsis and septic shock
Antibiotics should be administered within 1 hour of the identification of severe sepsis and septic shock, if possible, after obtaining appropriate cultures. The initial empiric antibiotic therapy should include one or more drugs that have activity against the likely pathogens and that penetrate the presumed source of sepsis. Initially, broad antibiotic coverage is recommended. Following are the general rules which can help for decision making:
Suggested initial empiric antimicrobial regimens based upon patient age, immunocompetence, and previous antibiotic administration include:
Children >28 days of age who are normal immunocompetent patient:
Children >28 days who are immunosuppressed or at risk for infection with Pseudomonas species:
Children who cannot receive penicillin or who have recently received broad-spectrum antibiotics:
a) Vancomycin/Teicoplanin plus Meropenem*
* Alternatives to Meropenam
Patients at increased risk of fungal infection (immunocompromised with persistent fever on broad spectrum antibiotics) or with an identified fungal source.
Add the following antifungals to the antimicrobial regimen
Patients with risk factors for rickettsial infection (eg, travel to or reside in an endemic region): Add a tetracyclin antibiotic (eg, doxycycline) to the antimicrobial regimen.
The empiric drug choice should be in accordance with the ongoing epidemic and endemic infections eg, H1N1, methicillinresistant S. aureus, chloroquine-resistant malaria, penicillin-resistant pneumococci.
Control of the Infection Source
The source of the infection should be located and treated early and aggressively. Conditions requiring debridement or drainage include necrotizing pneumonia, necrotizing fasciitis, gangrenous myonecrosis, empyema, and abscesses. Perforated viscus requires repair and peritoneal washout. If intravascular access devices are a possible source of severe sepsis or septic shock, they should be removed promptly after other vascular access has been established.
Duration of antibiotic therapy for sepsis
It will depend on the foci of infection, immune status of the patient and response to the antibiotics. If there are no complications the duration of therapy is 7-10 days. Longer courses may be appropriate in patients who have a slow clinical response, undrainable foci of infection, bacteremia with S. aureus; some fungal and viral infections or immunologic deficiencies, including neutropenia Use of procalcitonin levels or similar biomarkers may assist the clinician in the discontinuation of empiric antibiotics in patients.
Management of Central line/long line catheter-Related Infections -
1. Empirical coverage if suspecting gram-negative bacilli
Choice should be based on local antimicrobial susceptibility and the severity of disease a fourth-generation cephalosporin, carbapenem, or b-lactam/b-lactamase combination, with or without an aminoglycoside).
2. Empirical antimicrobial therapy if suspecting MRSA
3. Empirical combination antibiotic coverage for MDR gram-negative bacilli, such as Pseudomonas aeruginosa, should be used when CRBSI is suspected in
4. Empirical therapy for suspected CRBSI involving femoral catheters in critically ill patients should include coverage for gram-positive pathogens, gram-negative bacilli and Candida species.
5. Empirical therapy if catheter-related candidemia is suspected
*It should be suspected in septic patients with any of the following risk factors: total parenteral nutrition, prolonged use of broad-spectrum antibiotics, hematologic malignancy, receipt of bone marrow or solid-organ transplant, femoral catheterization, or colonization due to Candida species at multiple sites.
6. Antibiotic lock therapy should be used for catheter salvage; however, if antibiotic lock therapy cannot be used, systemic antibiotics should be administered through the colonized catheter.
Duration of antimicrobial therapy:
A. Uncomplicated Short term central venous or arterial catheter related blood stream infection
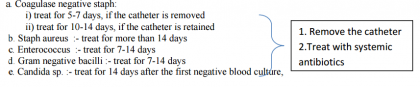
B. Complicated Short term central venous or arterial catheter related blood stream
Four to 6 weeks of antibiotic therapy should be administered to patients with persistent fungemia or bacteremia after catheter removal (i.e., occurring more than 72 hours after catheter removal), and to patients who are found to have infective endocarditis or suppurative thrombophlebitis, and to pediatric patients with osteomyelitis.
BRAIN ABSCESS
Inj Ceftriaxone + Vancomycin OR
Inj Teicoplanin + Metronidazole,
Drain pus, rationalize antibiotics according to culture and sensitivity and continue for 3 to 4 week
OSTEOMYELITIS-
Co-Amoxy clavulunic + Gentamicin
SEPTIC ARTHRITIS
TETANUS - Inj Crystalline Penicillin (2 lac IU /kg/ d /12 hourly) or Inj Metronidazole (mg/kg/d).
ACUTE ENDOCARDITIS - Inj Crystalline Penicillin/ampicillin + Gentamicin for 3-4 weeks is given which is tailored depending upon culture & sensitivity report.
MALARIA - As per National Malaria Control Program guidelines. See chapter 8.
UBERCULOSIS IN CHILDREN
Refer to RNTCP guidelines
ACUTE RHEUMATIC FEVER (ARF)
*Contraindicated in penicillin allergy
# maximum dose-500mg; contraindicated in liver disorders; can be given in patients with penicillin allergy; do not use if high rates of group A streptococal macrolide resistance prevalent.
Duration for secondary prophylaxis:
It depends on the presence of carditis during the acute episode.
PAEDIATRIC SURGICAL CASES
Specific Conditions
For Infant below 2 months age (more than 2kg):
| Antibiotic | Each dose | Frequency | Route | Duration |
| <7days >7days | ||||
| Inj. Cefotaxime + Inj. Gentamicin | 50 mg/kg/dose 5 mg/kg/dose | 12 hrly 8 hrly 24 hrly 24 hrly | IV IV | 2-3 weeks |
| 2nd line therapy: Meropenem+ Vancomycin | 20 mg/kg/dose 15 mg/kg/dose | 12 hly 8 hly 12 hly 8 hly | IV | 2-3 weeks |
- Treat bacterial meningitis due to Gram-negative bacilli or Staphyloccocus sp for at least 21 days.
For 2 months and above-
Inj Ceftriaxone (100mg/kg/day-2 divided dosage) for 10 -14 days
2nd line therapy: Meropenem (120 mg/kg/day in 3 div doses) + Vancomycin (60mg /kg/day in 4 div doses) for 10-14 days
- In case Ceftriaxone is not available, Inj Cefotaxime (200mg/kg/d, 3-4 divided doses) is given for the same duration.
- However if strong clinical suspicion for Staphylococcus infection in the form of skin boils, arthritis or flowing external wounds – Inj. Vancomycin can be added. In such situations the regimen is given for minimum period of 3 weeks.
- With confirmed meningococcal disease, treat with intravenous Ceftriaxone for 7 days.
- H influenzae type b meningitis is treated with intravenous Ceftriaxone for 10 days.
- S pneumoniae meningitis is treated with intravenous Ceftriaxone for 14 days.
- Bacterial meningitis due to Staphyloccocus sp is treated for at least 21 days.
Chemoprophylaxis for Meningococcal Disease Contacts (including non-vaccinated Hospital Staff): To be effective in preventing secondary cases, chemoprophylaxis must be initiated as soon as possible (i.e. not later than 48 hours after diagnosis of the case). Mass chemoprophylaxis not needed.
| Drug | Dose (Adults) | Dose (Children) | Route | Duration |
| Rifampicin | 600mg/12hr | 10mg/kg/12hr | Oral | Two Days |
| Ciprofloxacin | 500mg | - | Oral | Single Dose |
| Ceftriaxone | 250mg | < 15yr – 125mg | IM | Single Dose |
| Azithromycin | 500mg | 10mg/kg | Oral | Single Dose |
LOWER RESPIRATORY TRACT INFECTION-
Community acquired Pneumonia is categorized in to 2 types –Severe pneumonia (those with respiratory distress) and pneumonia (those with fast breathing only, treated on OPD basis).
For Severe Pneumonia (Children with respiratory distress requiring indoor care)-
- Under 2 months of age:
o Inj Cefotaxime / Ceftriaxone and Gentamicin for 10 days. - Over 2 months of age:
- Inj. Ampicillin (50mg/kg/dose 6h) + Gentamicin (7.5mg/kg/day OD i.m or i.v) is used. Inj Ampicillin can be switched to Oral Amoxycillin (45mg/kg/day TDS) once child is stable and able to take oral feeds. Total treatment duration is 7-10 days.
- In case of no response in 2 days the patient is assessed for complications like empyema, or infection at any other site. In the absence of any complication, a 3rd generation Cephalosporin (Cefotaxime 50mg/kg/dose 6h or Ceftriaxone 75- 100mg/kg/day in two divided doses, IV ) is used and can be switched to oral Cefopodoxime (10mg/kg/day BD) once the child is able to take orally. Total treatment duration is 7-10 days.
- In case the patient has severe sepsis/ septic shock, Inj. Piperacillin + Tazobactam (90mg/kg/dose 6h) + MRSA cover with IV Vancomycin (15mg/kg/dose 6h) is recommended.
Whenever Staphyloccus aureus is suspected in children (see Text Box), the various drug options are:
It is important to have high index of suspicion for staphylococcal infection as the initial choice of antibiotic does not cover this less common but a more severe infection adequately. Staphylococcal pneumonia is suspected if any child with pneumonia has:
To cover for staphylococcal infection, Cloxacillin or other antistaphyloccal drug should be added to the initial regimen as discussed in the text. |
- In severe pneumonia, use Inj.Cloxacillin or Inj Clindamycin may be added to the initial regime. OR
- Oral or IV Co- Amoxyclavulanic acid can be used.
- In very severe necrotizing pneumonia or for a patient in septic shock, MRSA cover should be added with IV Vancomycin Vancomycin 25-30 mg IV loading followed by 15-20 mg/kg 8-12 Hourly /)/ Teicoplanin 12 mg/kg x3 doses followed by 6 mg/kg once a day or Linezolid (10mg/kg/dose 8h).
- The total duration for treatment for uncomplicated Staphylococcal pneumonia is 3-4 weeks.
For pneumonia (OPD)
- Oral Amoxicillin (45mg/kg/day TDS) for a period of 5 days is recommended as the first choice. In case of non availability, one may use oral Co-trimoxazole (8mg/kg/day of TMP component BD).
Routine use of macrolide antibiotics for all cases of pneumonia is not advocated. Recent data suggests that (i) the routine addition of macrolides to children with CAP does not improve outcome (ii) selective use of macrolides would reduce their indiscriminate use and reduce antibiotic resistance.
Classically the mycoplasma pneumonia presents in an atypical fashion but literature suggests that it can sometimes be difficult to distinguish mycoplasma pneumonia from a pyogenic pneumonia.
Macrolide antibiotics should be considered in following clinical scenarios where the likelihood of mycoplasma pneumonia is high:
- Children with a subacute presentation with prolonged low grade fever, persistent cough, chest signs out of proportion to the radiographic abnormality (usually showing perihilar streaky infiltrates).
- Children with CAP (acute pneumonia like presentation with radiological evidence of patchy or lobar consolidation) who also have or develop extrapulmonary manifestations like myocarditis, hemolytic anemias, glomeruonephritis, aseptic arthritis, CNS problems (aseptic meningitis, encephalitis, ataxia), etc.
- Non response to first line antibiotics in children who are immunized with Hib/PCV and have no suppurative complications of CAP.
In the first two conditions macrolide antibiotics can be used along with the first line therapy for CAP.
EMPYEMA
- Proper drainage : Forms the main core of treatment.
Antimicrobial Therapy:
- Anti- Staphylococcal penicillin (Cloxacillin 100-200 mg/kg/day) along with 3rd generation cephalosporin like Ceftriaxone may be used as first line drug.
- Co-Amoxyclav is alternative first line therapy.
- In seriously ill patients with disseminated staphylococcal disease and septic shock to cover for MRSA, Vancomycin is recommended. Vancomycin is less effective than the first line drugs for the commoner Methicillin sensitive strains of Staphylococcus aureus.
- Children may continue to be febrile for 5-7 days after starting antibiotic therapy in the case of S. pneumoniae and H. influenzae and for 10-14 days in the case of Staphylococcus aureus. The clinical response to therapy should be assessed with parameters such decrease in fever, normalization of lab parameters such as CBC count, CRP, decrease in drain volume, clearing in chest x-ray, improvement in the overall condition of the patient.
- The decline in toxicity and fever are good signs of likely response. In case of complete non response after 96 hours of treatment, high spiking fever and persistent drainage, second line treatment may be instituted. Vancomycin should be substituted instead of the first line cloxacillin or co-amoxyclav.
- All children with non response should be evaluated for presence of pus pockets in the pleural cavity by an ultrasound chest. Here the key lies in better drainage rather than in a change of antibiotics. Extraneous causes of fever should also be evaluated.
VENTILATOR ASSOCIATED PNEUMONIA:
Treat as per the sensitivity pattern of your ICU.
General Suggestion:
| Potential Pathogens | Combination antibiotic therapy |
| Pseudomonas aeruginosa Or Klebsiella pneumonae (ESBL) Or Acinetobacter species | Beta Lactam + beta lactamase inhibitor (Piperacillin – Tazobactam) Plus Either Aminoglycoside (Amikacin, Gentamicin, or Tobramycin) OR Antipseudomonal fluroquinolone (Cipro/ Levofloxacin) |
| Methicillin – resistant Staphylococcus aureus (MRSA) | Vancomycin or Linezolid |
Second line Therapy
- Meropenem – 60 mg/kg/day I/V every 8 hrly AND Vancomycin - 40 mg/kg/day I/V every 6 - 8 hrly.
Third line Therapy
- Colistin base IV., 2.5 – 5 mg/kg/day I/V every 6 – 12 hrly (1mg= 30000 IU) AND Vancomycin - 40 mg/kg/day I/V every 6 - 8 hrly.
UPPER RESPIRATORY TRACT INFECTIONS
As these are mostly viral in origin, antibiotics are not needed barring following situations
Bacterial Pharyngotonsillitis (Group A Streptococcus)-
| Any of the following Antibiotic (route) | Children (<30kg) (days)><30kg) (days) | Children(<30kg) (days)>>30kg) (days) |
| Penicillin V (Oral) | 250 mg BID x 10 days | 500 mg BID x 10 days |
| Amoxycillin (Oral) | 40 mg/kg/day x 10 days | 250 mg TID, can be given BID |
| Benzathine Pencillin G (IM) | 6 Lakh units (Single Dose) | 12 Lakh units (Single Dose) |
While Penicillin is the drug of choice Amoxycillin is good alternative and used widely.
If the patient is Pencillin allergic, the alternative drugs are
| Antibiotic (route) | Dose and duration |
| Erythromycin (oral) | 40-50 mg/kg/day BID or TID x 10 days |
| Azithromycin (oral) | 12 mg/kg OD x 5 days |
| First Generation Cephalosporin (oral) (10 days) (if only, it is non Type 1 allergy to penicillin) | Cefaclor (20-40 mg/kg/d in 3 divided doses) / Cephalexin (50 mg/kg/d in 3 divided doses) |
Faucial diphtheria
- Inj.Crystalline Penicillin (100,000-150,000 Units/kg/day I.V 6h) for 10 days in recommended. Alternativey, Inj.Procaine Penicillin 25,000-50,000 U/kg/day BD maximum of 12 lakh units i.m. can be used.
- In case of penicillin allergy, Erythromycin (40-50mg/kg/day TDS/QID for 14 days or Azithromycin 10mg/kg/day OD for 5 days can be given.
Acute otitis media (AOM)-
- Oral Amoxicillin (45mg/kg/day TDS/50-60mg/kg/day in two divided doses) for 7 to 10 days is recommended.
- For severe cases (Severe Otalgia and/ or Temp >390C), Co-Amoxycillin Clavulanate (45 mg/kg/day po BD) or Inj.Ceftriaxone 75 mg/kg/day OD can be used.
- In case of penicillin allergy, Cefidinir (14 mg/kg/d in 2 divided doses) can be used.
- Total duration of treatment is recommended for 7 to 10 days.
Mastoiditis And Other Acute Ear Infection
- Inj. Amoxicillin-clavulanate OR 3rd Gen Cephalosporin (Ceftriaxone/ cefotaxime).
CSOM
- Routinely systemic antibiotic is not recommended until there is exacerbation and these are referred to ENT.
Acute Sinusitis with URI-
- Oral Amoxycillin (45 mg/kg/day TDS) for 7-10 days is recommended. For severe cases, Amoxycillin Clavulanate (45 mg/kg/day oral BD) or Inj.Ceftriaxone 75 mg/kg/day OD can be used.
Ludwig’s Angina
- 1st line : Clindamycin IV 8 hourly or Amoxicillin-Clavulanate IV.
- 2nd line : Piperacillin-Tazobactam IV 6 hourly.
Pertussis
- Erythromycin for 14 days, Azithromycin for 5 days, Clarithromycin for 7 days and have similar efficacy but differ in terms of cost, duration of therapy, side effects, tolerability, likelihood of drug interaction. Considering all factors, Azithromycin in a dose of 10 mg/kg once a day for 5 days in infants less than 6 months and 10 mg/kg on day 1 and then 5 mg/kg day on 2 to 5 days is the cheapest, shortest best tolerated and most convenient option and can be safely given to infants less than 1 month (unlike all other macrolides).
GASTRO-INTESTINAL DISEASES
Dysentery
(a) For inpatients- Inj Ceftriaxone (100mg/kg) for 5-7 days.
(b) For OPD cases
- Cefixime (8mg/kg/day BD)
Or
Azithromycin 10-20 mg/ kg (ceiling dose of 1 gm) for 5 days. - In case of non response after 2 antibiotics, investigate for appropriate therapy. Fluoroquinolones are not preferred due to high level of resistance in many parts of the country.
Cholera
- Single dose oral azithromycin 10 mg/ kg (ceiling dose of 1 gm) or Doxycycline (50mg for less than 3 years and 100 mg for those above).
Enteric Fever
(a) For OPD cases-
- Oral Cefixime 20 mg/kg/day (max dose of 1200) for 14 days or azithromycin 10-20 mg/kg (ceiling dose of 1 gm) for 7-10 days. Antibiotic therapy should be continued till one week post-fever defervescence.
(b) For inpatients
- Inj Ceftriaxone 100 mg/ kg/day and shift to oral cefixime once fever resolves. Antibiotic therapy should be continued till one week post-fever defervescence.
- Second line:
a) Ofloxacin 15mg/kg/d in two divided doses for 10-14 days. Antibiotic therapy should be continued till one week post-fever defervescence.
b) Chloramphenicol (50- 75mg/kg/day PO) x 14 days.
c) TMP-SMX (8 mg/kg/day of TMP PO) x 14 days.
Peritonitis
For primary peritonitis in nephrotic syndrome: Inj. Ampicillin + Aminoglycoside OR inj. cefotaxime for primary peritonitis in a cirrhotic, inj. cefotaxime.
Liver Abscess
| 1st Line | 2nd Line | |
| Amoxycillin-clavulanate/ 3rd generation cephalosporin + Aminoglycoside Metronidazole (30-50 mg/kg/d in 3 divided doses for 10-14 days) is added if Amoebic abscess suspected | Piperacillin- Tazobactam IV | Ultrasound guided drainage indicated in large abscesses, signs of imminent rupture and no response to medical treatment. |
Total duration of therapy is 4-6 weeks
URINARY TRACT INFECTION (UTI)
a) Uncomplicated UTI (age> 2 months with lower UTI, without any urinary tract obstruction) -
Oral Cotrimoxazole (8-10mg of TMP component) /kg/day oral BD
OR
Cefixime (8-10 mg/kg/day BD) to be given for 7-10 days
OR
Co Amoxycillin+Clavulanic Acid (30-50 mg of Amoxicillin) for 7-10 days.
b) Complicated / Severe UTI (Febrile UTI, Systemic toxicity, renal angle tenderness or with any urinary structural abnormality) and all UTI in children less than 2 months should be treated with parenteral antibiotics.
Inj. Cefotaxime (150-200mg/kg/day 8h OR
Inj. Ceftriaxone (100mg/kg/day OD OR
Inj. Amikacin 15mg/kg OD
To be given for 10-14 days
c) In Immunocompromised host/ severe systemic sepsis or as second line for complicated UTI-
Inj. Piperacillin Tazobactum 90mg/kg/dose IV 6h) or Inj. Meropenem (20-40mg/kg/dose 8h) To be given for 10-14 days
FEBRILE NEUTROPENIA
| 1st Line | 2nd Line | 3rd Line |
| Ceftazidime (150 mg/kg/day in 3div doses)+ Amikacin (15- 20mg/kg/day in 2 or 3 div doses) | Piperacillin + Tazobactam (200- 300 mg/kg/day IV in 3-4 div doses)+ Vancomycin (40 mg/kg/day IV in 4 divided doses) | Meropenem (60 mg/kg/day in 3 div doses) + Amphotericin B (1 mg/kg/day IV for 2 weeks) or liposomal Amphotericin B 1-5 mg kg/day, usually 3 mg/kg/day |
- Patients without an identified etiology who become afebrile within first 3-5 days of therapy and are clinically well with ANC of > 200 cells/cmm can be shifted to oral antibiotics (Cefixime or Co- Amoxy- Clavulanic acid) and therapy should be continued for minimum 7 days.
- However, if fever persists or ANC remains <200 parenteral therapy should be continued with 2nd line antibiotics.
- In clinically stable patients without an identified etiology but with persistent neutropenia, therapy can be stopped after 2 weeks.
Presumptive therapy for initial antimicrobial coverage in critically ill children with severe sepsis and septic shock
Antibiotics should be administered within 1 hour of the identification of severe sepsis and septic shock, if possible, after obtaining appropriate cultures. The initial empiric antibiotic therapy should include one or more drugs that have activity against the likely pathogens and that penetrate the presumed source of sepsis. Initially, broad antibiotic coverage is recommended. Following are the general rules which can help for decision making:
- All children with septic shock should receive coverage for methicillin-resistant Staphylococcus aureus (MRSA) initially at recognition of the event.
- Coverage for enteric organisms should be added whenever clinical features suggest genitourinary and/or gastrointestinal sources (eg, perforated appendicitis or bacterial overgrowth in a child with short gut syndrome).
- Treatment for Pseudomonas species should be included for children who are immunosuppressed or at risk for infection like those with cystic fibrosis).
- When treating empirically, antibiotics which can be given by rapid intravenous bolus (eg, beta-lactam agents or cephalosporins) should be administered first followed by infusions of antibiotics, such as vancomycin, that must be delivered more slowly.
- Ongoing antimicrobial therapy should be modified based upon culture results, including antimicrobial susceptibility and the patient's clinical course.
Suggested initial empiric antimicrobial regimens based upon patient age, immunocompetence, and previous antibiotic administration include:
Children >28 days of age who are normal immunocompetent patient:
- Ceftriaxone/Cefotaxime plus Vancomycin //Teicoplanin
- Consider adding an aminoglycoside (eg, gentamicin/amikacin) if possibility of genito- urinary source is likely
- Consider adding piperacillin-tazobactam / clindamycin / metronidazole if possibility of gastro-intestinal source.
Children >28 days who are immunosuppressed or at risk for infection with Pseudomonas species:
- Ceftazidime or Cefepime plus Vancomycin/Teicoplanin.
- add an aminoglycoside or carbapenem in settings where bacterial organisms with extended-spectrum beta-lactamase (ESBL) resistance are prevalent.
- addition of a carbapenem is favored over an aminoglycoside if the patient has received any broad-spectrum antibiotics like 3 rd generation cephalosporin, aminoglycoside or fluoroquinolone within two weeks.
Children who cannot receive penicillin or who have recently received broad-spectrum antibiotics:
a) Vancomycin/Teicoplanin plus Meropenem*
* Alternatives to Meropenam
- Aztreonam OR
- Ciprofloxacin plus Clindamycin
Patients at increased risk of fungal infection (immunocompromised with persistent fever on broad spectrum antibiotics) or with an identified fungal source.
Add the following antifungals to the antimicrobial regimen
- Liposomal Amphotericin B or
- an echinocandin (eg, caspofungin, micafungin)
Patients with risk factors for rickettsial infection (eg, travel to or reside in an endemic region): Add a tetracyclin antibiotic (eg, doxycycline) to the antimicrobial regimen.
The empiric drug choice should be in accordance with the ongoing epidemic and endemic infections eg, H1N1, methicillinresistant S. aureus, chloroquine-resistant malaria, penicillin-resistant pneumococci.
Control of the Infection Source
The source of the infection should be located and treated early and aggressively. Conditions requiring debridement or drainage include necrotizing pneumonia, necrotizing fasciitis, gangrenous myonecrosis, empyema, and abscesses. Perforated viscus requires repair and peritoneal washout. If intravascular access devices are a possible source of severe sepsis or septic shock, they should be removed promptly after other vascular access has been established.
Duration of antibiotic therapy for sepsis
It will depend on the foci of infection, immune status of the patient and response to the antibiotics. If there are no complications the duration of therapy is 7-10 days. Longer courses may be appropriate in patients who have a slow clinical response, undrainable foci of infection, bacteremia with S. aureus; some fungal and viral infections or immunologic deficiencies, including neutropenia Use of procalcitonin levels or similar biomarkers may assist the clinician in the discontinuation of empiric antibiotics in patients.
Management of Central line/long line catheter-Related Infections -
1. Empirical coverage if suspecting gram-negative bacilli
Choice should be based on local antimicrobial susceptibility and the severity of disease a fourth-generation cephalosporin, carbapenem, or b-lactam/b-lactamase combination, with or without an aminoglycoside).
2. Empirical antimicrobial therapy if suspecting MRSA
- for health care settings with an elevated prevalence of MRSA- Vancomycin is recommended.
- for institutions in which the most of MRSA isolates have vancomycin minimum inhibitory concentration (MIC) values 12 mg/mL- Daptomycin, should be used.
- Linezolid should not be used for empirical therapy.
3. Empirical combination antibiotic coverage for MDR gram-negative bacilli, such as Pseudomonas aeruginosa, should be used when CRBSI is suspected in
- Neutropenic patients
- severely ill patients with sepsis
- patients known to be colonized with such pathogens, until the culture and susceptibility data are available and deescalation of the antibiotic regimen can be done.
4. Empirical therapy for suspected CRBSI involving femoral catheters in critically ill patients should include coverage for gram-positive pathogens, gram-negative bacilli and Candida species.
5. Empirical therapy if catheter-related candidemia is suspected
- Echinocandin or
- Fluconazole can be used in patients without azole exposure in the previous 3 months in health care settings where the risk of Candida krusei or Candida glabratainfection is very low.
*It should be suspected in septic patients with any of the following risk factors: total parenteral nutrition, prolonged use of broad-spectrum antibiotics, hematologic malignancy, receipt of bone marrow or solid-organ transplant, femoral catheterization, or colonization due to Candida species at multiple sites.
6. Antibiotic lock therapy should be used for catheter salvage; however, if antibiotic lock therapy cannot be used, systemic antibiotics should be administered through the colonized catheter.
Duration of antimicrobial therapy:
A. Uncomplicated Short term central venous or arterial catheter related blood stream infection
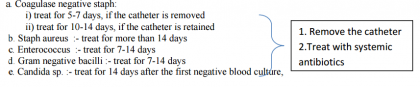
B. Complicated Short term central venous or arterial catheter related blood stream
Four to 6 weeks of antibiotic therapy should be administered to patients with persistent fungemia or bacteremia after catheter removal (i.e., occurring more than 72 hours after catheter removal), and to patients who are found to have infective endocarditis or suppurative thrombophlebitis, and to pediatric patients with osteomyelitis.
BRAIN ABSCESS
Inj Ceftriaxone + Vancomycin OR
Inj Teicoplanin + Metronidazole,
Drain pus, rationalize antibiotics according to culture and sensitivity and continue for 3 to 4 week
OSTEOMYELITIS-
Co-Amoxy clavulunic + Gentamicin
SEPTIC ARTHRITIS
- 1 st line Inj Co-Amoxy clavulunic + Gentamicin
- 2nd line Inj Ceftriaxone//cefotaxime +/- Vancomycin
TETANUS - Inj Crystalline Penicillin (2 lac IU /kg/ d /12 hourly) or Inj Metronidazole (mg/kg/d).
ACUTE ENDOCARDITIS - Inj Crystalline Penicillin/ampicillin + Gentamicin for 3-4 weeks is given which is tailored depending upon culture & sensitivity report.
MALARIA - As per National Malaria Control Program guidelines. See chapter 8.
UBERCULOSIS IN CHILDREN
Refer to RNTCP guidelines
ACUTE RHEUMATIC FEVER (ARF)
| Antibiotic | Dose | Route | Frequency | Duration | |||||
| Primary prophylaxis for rheumatic fever (Treatment of group A streptococcal tonsillo-pharyngitis) The primary goal of treating an ARF attack is to eradicate streptococcal organisms and bacterial antigens from the pharyngeal region. The antibiotic therapy is very effective if started within 9 days after onset of symptoms to prevent rheumatic fever specially carditis | |||||||||
| Benzathine Penicillin G* [After sensitivity testing] According to weight of the child | weight ≥ 27 kg :- 1.2 million units weight < 27 kg :- 0.6 million units | Deep intramuscular injection | Only once Single dose | Single dose | |||||
| Alternative antibiotics | |||||||||
| Azithromycin | 12.5 mg/kg/day divided | Oral | OD | 5 days | |||||
| Amoxicillin | 25–50mg/kg/day divided Adult dose 750-1500 mg/day | Oral | TDS | 10 days | |||||
| Cephalexin | 15-20 mg/kg/dose | Oral | BD | 10 days | |||||
| Erythromycin | 250 mg #OR 40 mg/kg/day divided | Oral | QID | 10 days | |||||
| Penicillin-V | 250 mg Adult dose 500mg | Oral | QID | 10 days | |||||
| Secondary prophylaxis for rheumatic fever It involves continuous administration of antibiotics in patients with a previous attack of RF and/or rheumatic heart disease. It is mandatory for all patients who have had an attack of RF, whether or not they have residual rheumatic valvular heart disease | |||||||||
| Benzathine Penicillin G | Same as above | same | same | Every 3-4 weeks | |||||
| Penicillin V | Same | same | BD | See below | |||||
| Sulfadiazine (patients allergic to penicillin) | weight >27 kg:- 0.5 g weight ≥27 kg:- 1 g | oral | OD | See below | |||||
| Erythromycin (patients allergic to penicillin & sufadiazine) | Same | same | BD | See below | |||||
*Contraindicated in penicillin allergy
# maximum dose-500mg; contraindicated in liver disorders; can be given in patients with penicillin allergy; do not use if high rates of group A streptococal macrolide resistance prevalent.
Duration for secondary prophylaxis:
It depends on the presence of carditis during the acute episode.
- NO carditis: continue for 5 years after last attack or 18 years of age [whichever is longer].
- Carditis present (healed carditis or mild mitral regurgitation): continue for 10 yearsafter last attack or 25 years of age [whichever is longer]
- Carditis present (established heart disease or following valve surgery or ballon mitral valvotomy): continue lifelong.
- Expert consultation should be sought if want to discontinue after 40 years of age instead of life-long prophylaxis as recurrence beyond this age is minimal.
PAEDIATRIC SURGICAL CASES
| Clean Surgery | Clean Surgery likely to be contaminated | Contaminated/dirty Surgery or Peritonitis |
| Surgeries like Uncomplicated Hernia, cyst excision, hydrocoele - No Pre-operative prophylaxis needed For all other surgeries under this group: Inj Ceftriaxone 50 – 75 mg/kg/day I.V or I/M single dose half an hour before surgery | For GI surgeries Inj Ceftriaxone 50 – 75 mg/kg/day, I.V or I/M 12 hly doses AND Metronidazole 20 – 30 mg/kg/day I/V every 8 hrly Given for 48hrs only. Urinary tract surgeries Inj Ceftriaxone 50 – 75 mg/kg/day I.V or I/M 12hrly doses Do not continue beyond 48hrs of surgery | All surgeries under this group Inj Ceftriaxone 50 – 75 mg/kg/day, I.V or I/M 12hrly doses AND Metronidazole 20 – 30 mg/kg/day I/V every 8 hrly AND Gentamicin 7.5mg/kg/d 24hrly IV or IM 2nd Line Piperacillin + Tazobactam (200-300 mg/kg/day IV in 3-4 div doses) + Vancomycin (40 mg/kg/day IV in 4 divided doses) |
| Cellulitis/ Abscesses | Cloxacillin (50- 100 mg/kg/d) in 3-4 divided doses OR Co- AmoxyClav OR Cefazolin (50 mg/Kg/d in 6-8 h doses | Clindamycin (20- 40mg/Kg/d in 6-8 hly doses) | Treat for 5-7 days. |
Directorate General of health servicesGovernment of IndiaguidelinesMinistry of Health & Family WelfareNational Centre For DiseasePediatric Infectionstreatment guidelines
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd