- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Fracture of shaft of the humerus - Standard Treatment Guidelines
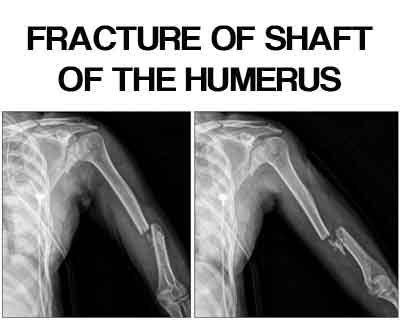
The Ministry of Health and Family Welfare has issued the Standard Treatment Guidelines Critical Care for Fracture of Shaft Of The Humerus. Following are the major recommendations:
Incidence :
Fractures of the humeral shaft account for roughly 3% of all fractures.
Classification :
AO Classification :
Bone = humerus = 1
Segment = diaphysis = 2
Groups = A/B/C where
A: Simple fracture
B: Wedge fracture
C: Complex fracture
Subgroups:
A1: Simple fracture, spiral
A2: Simple fracture, oblique (≥30deg)
A3: Simple fracture, transverse (<30deg)
B1: Wedge fracture, spiral wedge
B2: Wedge fracture, bending wedge
B3: Wedge fracture, fragmented wedge
C1: Complex fracture, spiral
C2: Complex fracture, segmental
C3: Complex fracture, irregular
History :
Fall from a height or a direct impact as in vehicular accidents.
Diagnosis :
- Swelling, pain and bruising are common features.
- The arm may appear shortened and deformed if the fracture is significantly displaced.
- Inability to extend the wrist (wrist drop) and sensory deficit over the base of the thumb on the dorsal aspect indicates an associated injury of the radial nerve.
- A thorough assessment of the peripheral neurovascular status is essential in all humeral shaft fractures.
- Associated injuries to the shoulder and elbow joints are not uncommon.
- X-rays (AP and lateral) of the entire humerus including the shoulder and elbow joint should be taken to confirm the diagnosis.
- CT is rarely indicated.
Complications :
- Nerve injury - Radial nerve palsy (upto 10%) is the most important complication.
- Vascular injury - Injuries to the brachial artery have been reported in association with humeral shaft fractures. A careful assessment of the peripheral circulation is essential in all humeral fractures.
- Non-union - In general, spiral or oblique fractures heal better than the transverse or segmental fracture. Soft tissue interposition, excessive fracture mobility and infection are important factors responsible for non-union of a humeral shaft fracture.
- Joint stiffness - A proper rehabilitation programme is essential to prevent joint stiffness following injury.
- Malunion - This may be functionally inconsequential; arm musculature and shoulder, elbow, and trunk range of motion can compensate for angular, rotational, and shortening deformities.
Investigations :
- AP and lateral radiographs of the humerus should be obtained, including the shoulder and elbow joints on each view. ,
- Traction radiographs may aid in fracture definition in cases of severely displaced or comminuted fracture patterns.
- Computed tomography, bone scans, and MRI are rarely indicated except in cases in which pathologic fracture is suspected.
Management :
- Conservative :
- Most humeral shaft fractures (>90%) will heal with nonsurgical management.
- Twenty degrees of anterior angulation, 30 degrees of varus angulation, and up to 3 cm of bayonet apposition are acceptable and will not compromise function or appearance.
- Hanging cast: This utilizes dependency traction by the weight of the cast and arm to effect fracture reduction.
- Indications include displaced midshaft humeral fractures with shortening, particularly spiral or oblique patterns. Transverse or short oblique fractures represent relative contraindications because of the potential for distraction and healing complications.
- The patient must remain upright or semi upright most of the time with the cast in a dependent position for effectiveness.
- It is frequently exchanged for functional bracing 1 to 2 weeks after injury.
- More than 90% union is reported
Operative :
Indications for operative treatment are:
- Multiple trauma
- Inadequate closed reduction or unacceptable malunion
- Pathologic fracture
- Associated vascular injury
- Floating elbow
- Segmental fracture
- Intraarticular extension
- Bilateral humeral fractures
- Open fracture
- Neurologic loss following penetrating trauma
- Radial nerve palsy after fracture manipulation (controversial)
- Nonunion
Open reduction and internal fixation
The fracture site is exposed, fragments reduced and fixed with a compression plate (DCP, LCDCP, LCP) and screws, with an anterolateral approach or upper two thirds fracture and posterior approach for lower thirds fracture
Interlocking intramedullary nail
An ‘antegrade’ or a ‘retrograde’ nail is introduced into the medullary cavity of the humerus after closed reduction of the fracture. The nail is then locked proximally and distally to achieve rotational stability. This requires image intensification and is comparable to plating.
External fixation
This method of treatment may be used in open or multiple fractures. Percutaneous pins are threaded into the bone and then held together by an external frame.
Patients with associated neurovascular injury or in unstable fractures where facilities are not available for ideal internal fixation should be referred to higher centre.
Comments :
The common deficiency
(i) The writing style is not consistent. Radial head fracture is given as 33% of elbow region while distal radius as 1/6 of fracture (not known) of what?
(j) Imaging – just mentioned AP, Lateral and sometime oblique. Why and for what a particular special x-ray is needed?
(k) Complication has been clubbed as most common to least common, early or late in one list. This will not help.
(l) When to refer – Generally written type B & C to higher center. Can we make such guidelines in the issue.
The outcome of treatment depends on –
e) Training of the surgeon.
f) Infrastructure – operating theatre & available instrumentation
We need to define what all we should have in primary health center, secondary and tertiary care centre. If we refer all type B & C fracture for all fractures than how the patients in Village, Tehsil, District will be treated as we do not have any networking of referral centers (they are all concentrated in the cities.
Summarily the objective of the guidelines should be well stated. Is it to stop small centers in cities to stop operating the particular type of fractures and force them to refer or to make a national policy for the overall effective management of the orthopaedic patients?
Guidelines by The Ministry of Health and Family Welfare :
Group Head Coordinates of Development Team Dr. P.K. DAVE, Rockland Hospital, New Delhi Dr. P.S. Maini, Fortis Jessa Ram Hospital, New Delhi
Reviewed By
Dr. V.K. Sharma, Professor Central Instiute of Orthopaedics, Safdarjung Hospital, New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd