- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Fish bone pierces intestine and causes abdominal wall abscess: rare case
Dr Kiyomitsu Kuwahara at the Department of Surgery, Yachiyo Hospital, Anjo-shi, Aichi, Japan and colleagues have reported a rare case of Fishbone piercing intestine and causing abdominal wall abscess.The case has appeared in the Journal of Medical Case Reports.
Foreign body ingestion sometimes occurs accidentally and is usually related to food, such as fish and chicken bones, and includes ingestion of toothpicks. A small percentage of patients with foreign body ingestion develop complications, which have a variety of clinical presentations. Less than 1% of cases require surgical intervention.
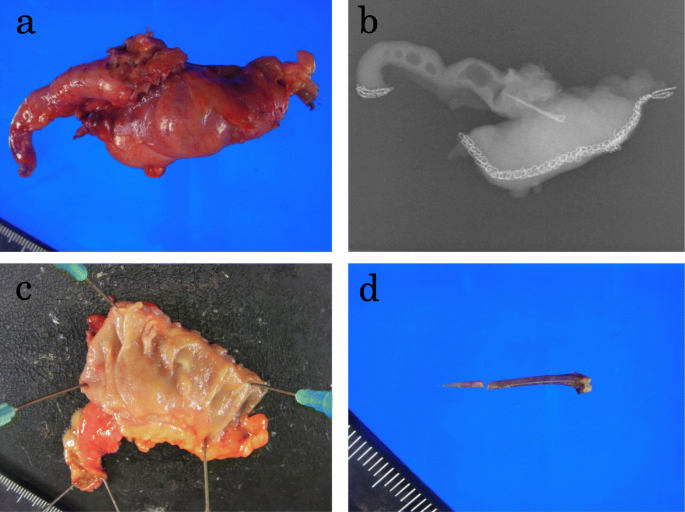
A 55-year-old Japanese man presented to our hospital with a complaint of right lower abdominal pain. His medical and family histories were unremarkable. He worked in a factory. He occasionally consumed alcohol and smoked cigarettes. He denied having eaten fish during the previous few days. Three days prior to visiting the hospital, he noticed the redness of the skin and pain involving his right lower abdomen. A physical examination revealed tenderness, swelling, and redness at the right iliac fossa; however, he was afebrile (36.5 °C). His blood pressure and pulse were 122/80 mmHg and 85 beats per minute (bpm), respectively. A laboratory examination revealed an increased white blood cell (WBC) count of 10.4 × 103 cells/μL and C-reactive protein (CRP) level of 10.19 mg/dL. Except for this finding, laboratory testing revealed no abnormal values. Computed tomography (CT) showed a 42 × 22 mm low-density area with rim enhancement in his right internal oblique muscle (Fig. 1a), and a 20 mm-long hyperdense, sharply pointed object in the wall of his cecum adjacent to the low-density area (Fig. 1b). Although he was unaware of having ingested a sharply pointed object such as a fishbone, we suspected that the object was a fishbone because of the shape. Thus, the findings were diagnosed as abdominal wall abscess due to a foreign body piercing the cecum. The abscess was aspirated but did not return fluid. A blood culture had no growth.
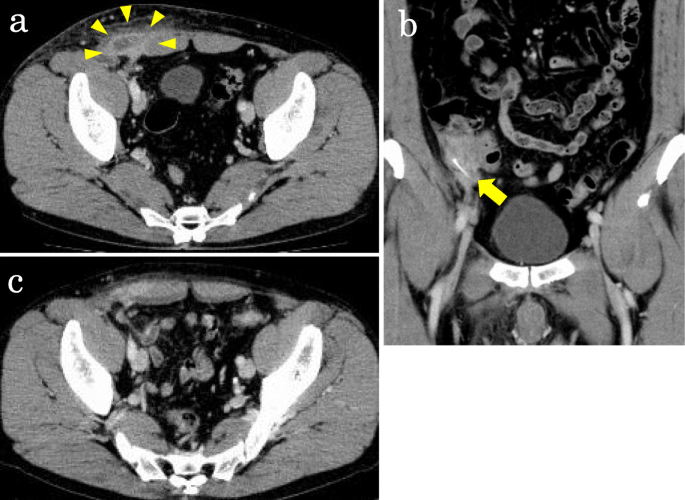
He was treated conservatively with flomoxef (2 g/day) for 2 weeks. After the treatment, his WBC and CRP level returned to normal, and the abdominal wall abscess was not seen on CT (Fig. 1c). His symptoms of tenderness, swelling, and redness at the right iliac fossa also improved. The hyperdense pointed object remained in the same location. Therefore, 24 days after the diagnosis, he underwent colonoscopy for removal of the object; however, no abnormality was visualized in his cecum. Although surgical removal was indicated, we monitored our patient carefully without performing surgery, based on a mutual agreement with our patient.
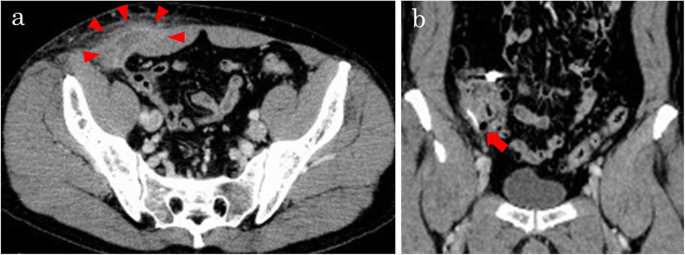
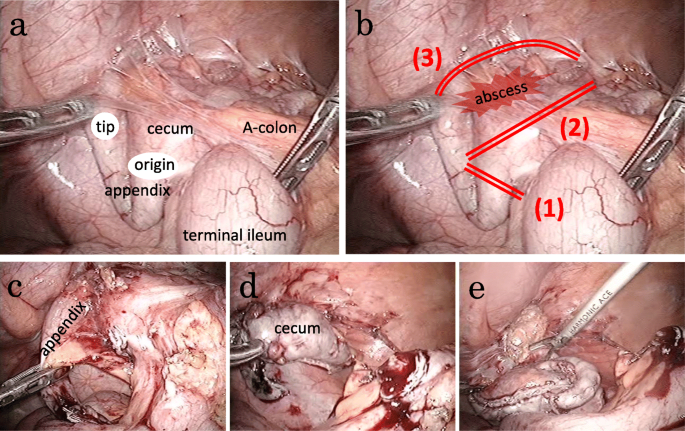
Two months after the initial treatment, he presented again with right lower abdominal pain. CT showed the same low-density area and the foreign body in the same location in the cecum (Fig. 2a, b); the findings were diagnosed as recurrence of the abdominal wall abscess due to the foreign body. Laparoscopic surgery was performed to remove the object. He was treated with flomoxef (2 g/day) for 7 days before laparoscopic surgery, and a subsequent laboratory examination revealed that his CRP level had decreased from 8.57 to 0.82 mg/dL. When he presented immediately before undergoing surgery, he no longer complained of right lower abdominal pain.
Journal of Medical Case Reports
For more details click on the link: https://doi.org/10.1186/s13256-019-2301-7

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd