- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Fetal MRI can reliably spot holoprosencephaly as early as 18 gestational weeks
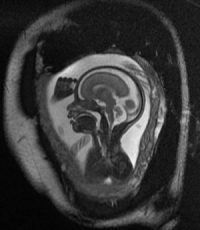
Fetal magnetic resonance imaging (MRI) can reliably spot holoprosencephaly as early as 18 gestational weeks, providing an opportunity to counsel families earlier in their pregnancy, according to Children's-led research published online May 18, 2018, in the American Journal of Medical Genetics. Accurately diagnosing holoprosencephaly is vital because the degree of severity of the brain malformation correlates with heightened risk of fetal and neonatal demise and intellectual disability among surviving children, the study authors write.
One of a series of fetal and postnatal MRI images captured by Children's National Health System faculty is featured on the journal's cover.
By about week five to six of pregnancy, the embryonic forebrain (prosencephalon) cleaves into two cerebral hemispheres. Holoprosencephaly is the incomplete separation of those cerebral hemispheres and occurs in 1.2 to 2.2 of every 10,000 live births. The brain defect is associated with genetic and environmental risk factors, including gestational diabetes, lower education level and aspirin use during pregnancy.
According to the study team, an expanded spectrum of holoprosencephaly disease phenotypes and milder variants have been identified, including:
- Aprosencephaly/atelencephaly, considered the most severe form, which can be accompanied by a range of facial deformities.
- Alobar, a variant that is associated with a single, midline forebrain and a holosphere shaped like a pancake, cup or a ball.
- Middle interhemispheric, which is marked by normal separation of the frontal and occipital poles but lack of separation in portions of the more posterior aspects of the frontal lobes and parietal lobes. Craniofacial defects have not been described in patients with this variant.
- Semilobar, which occurs when the anterior aspect of the cerebral hemispheres do not separate while some portions of the posterior hemispheres show separation. The noncleaved frontal lobes are usually small. Craniofacial defects are usually less severe than what is seen with the alobar variant.
- Lobar, which is characterized by less severe anatomical brain defects than the alobar and semilobar variants. Typically more than half of the total volume of the frontal lobes should be separated to qualify as lobar holoprosencephaly.
Ultrasound can diagnose the most severe forms of holoprosencephaly based on abnormal facial features, among other findings. For instance, fetal sonography can detect facial abnormalities associated with holoprosencephaly, such as lateral facial cleft.
However, some prenatal ultrasounds do not clearly distinguish between severe holoprosencephaly and other brain abnormalities, such as an excess accumulation of cerebrospinal fluid (severe hydrocephalus). While ultrasounds can provide more clarity by 24 weeks gestation, that leaves families little time to develop multidisciplinary care plans for infants likely to be born with complex care needs.
"Using fetal MRI, holoprosencephaly and its severity can be accurately established by 18 weeks of gestation and, in some cases, in fetuses as young as 16 weeks," says Youssef A. Kousa, M.S., D.O., Ph.D., a child neurology fellow at Children's National and the study's lead author. "Because of the strong link between the severity of brain abnormality and clinical outcomes, such early and accurate imaging is important for counseling families. Our findings and our detailed descriptions of the differences between disease variants should help to inform these important conversations during complicated pregnancies."
For more details click on the link: http://dx.doi.org/10.1002/ajmg.c.31618

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd