- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
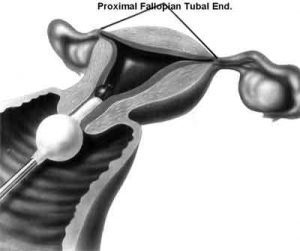
Fallopian Tube Recanalization in Infertility Due to Proximal Tubal Obstruction-Standard Treatment Guidelines
Infertility is defined as the inability to conceive after 1 year of contraceptive-free intercourse. Since the reasons for infertility may be due to multiple factors, a systematic approach is required diagnosis and management. It may be due to factors relating to fallopian tubes in 30-40%, mucus hostile to sperms in 15-20% and factors relating to males in 40% (1).
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Fallopian Tube Recanalization in Infertility Due to Proximal Tubal Obstruction.
Following are the major recommendations :
Introduction
A large number of pathologic conditions can affect the proximal fallopian tube . Infection and subsequent inflammation or fibrosis is leading causes of proximal tubal obstruction. These are frequently consequent to chlamydial or gonococcal salpingitis or postpartum endometritis. About half of patients with bilateral proximal tubal obstruction (PTO)have very localized disease with no pelvic adhesions (2,3), making them ideal candidates for an attempt at tubal catheterization for establishing patency. Moreover, PTO often occurs because of the accumulation of mucus or debris, which forms an impacted plug in the interstitial or proximal isthmic portion of the tube . fallopian tube recanalization (FTR) is a minimally invasive procedure used to recanalize blocked fallopian tubes in patients with a history of infertility and confirmed proximal tubal obstruction.
Case definition
For both situations of care (mentioned below*) Proximal tubal obstruction is defined as obstruction in either the intramural segment or the uterotubal junction, diagnosed as cornual block on hysterosalpingogram with normal fallopian tubes on , hysterocoposy or laparoscopy during work up of female infertility.
INCIDENCE OF THE CONDITION IN OUR COUNTRY
The exact incidence of female infertility due to proximal tubal disease in our country is not known. The incidence in United states has been reported to be 15-20%.In India, proximal tubal obstruction due to tubal spasm or transient occlusion by mucus plugs or debris has been reported in 10-40% of women in 2009(4,5).
DIFFERENTIAL DIAGNOSIS
Proximal, distal and peritubal damage can be caused by a number of disease processes, such as inflammation, endometriosis and surgical trauma . Bacteriological examination of tubal fluid detects pathologic micro flora in the oviducts of 36.6% women with PTO. Most common cause of fallopian tube obstruction is infection such as pelvic inflammatory disease (PID). The tubal infertility has been reported to be around 12% after one, 23% after two, and 53% after three episodes of PID (6). Inflammatory etiology seems to be important in isthmic tubal occlusion, especially due to chlamydial infection which causes muscular hypertrophy leading to salpingitis isthmica nodosa. Other factors such as uterine curettage, pelvic inflammatory disease, endometritis, infections after childbirth or abortions and intraabdominal infections including appendicitis and peritonitis and intrauterine devices may all influence PTO infertility .
PREVENTION AND COUNSELING
(a)Awareness about sexually transmitted infections and its early treatment.
Since tubal infertility may be the consequence of chronic pelvic inflammatory disease (PID), which can lead to tubal scarring. The latter can be prevented by early detection and treatment of sexually transmitted infections particularly Chlamydia infection (7).
(b)Avoidance of tobacco , smoking and obesity.
These lifestyle factors can cause fertility impairment during the reproductive years (8). Tobacco products not only cause infertility but also interfere with its treatment (8). Hence tobacco screening and cessation is an important component of infertility care (9). Obesity may be associated with ovulatory and menstrual dysfunction and subsequent infertility, increased risk of miscarriage, and decreased effectiveness of Assisted Reproductive Therapy (10).
(c)Regular treatment.
Proper & regular of the metabolic disorder associated with the polycystic ovary syndrome due to the link between overeating, insulin resistance, and the endocrine changes that reduce fertility in women with polycystic ovary syndrome (11).
(d) Avoidance of excessive and repeated exposure to radiation
(e)Proper diet and exercise. Optimal reproductive functioning requires both proper diet and appropriate levels of exercise. Women who are significantly overweight or underweight may have difficulty in becoming pregnant.
(f) Assisted reproductive therapy (ART)- In cases, where tubal recanalization is not possible in spite of various techniques, couples should be advised for Assisted reproductive therapy (ART).
OPTIMAL DIAGNOSTIC CRITERIA, INVESTIGATIONS, TREATMENT & REFERRAL CRITERIA
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis-Women with unilateral or bilateral proximal tube obstruction confirmed by hysterosalpingography (HSG) or laparoscopy are candidates for fallopian tube recanalization. Proper historical evaluation, general physical and gynaecological examination and exclusion of infective etiology should precede (HSG).
Investigations-
Sonography
Sonography should be performed for evaluation of uterus and adnexae to exclude uterine abnormalities, hydrosalpinx, polycystic ovaries, endometriosis and fluid in Pouch of Douglas.
Hysterosalpingography (HSG)
Hysterosalpingography (HSG) should be performed to demonstrate endometrial cavity, uterine abnormalities, fallopian tubes with peritoneal spill, level of blockage(proximal, mid or distal) in case of blocked fallopian tubes, presence or absence of hydrosalpinx. About 10% of patients with apparent bilateral blocked fallopian tubes on HSG become pregnant without further therapy and may demonstrate patent tubes on repeat HSG. However, HSG is contraindicated in acute pelvic inflammatory disease, active uterine bleeding, recent curettage and intrauterine adhesions.
Diagnostic criteria of PTO
Hysterosalpingography shows persistent unilateral or bilateral tubal occlusion in spite of administration of anticholinergic drugs or spasmolytics.
Treatment:
Standard Operating procedure
a. In Patient- This is not applicable as admission is not required for these investigations.
b. Out Patient- Sonography and HSG are performed as OPD procedures
c. Day Care- This is not applicable as admission is not required for these investigations.
Referral criteria:
Infertile women with detection of persistent unilateral or bilateral proximal tubal obstruction within the first 0-4 cm of the fallopian tube on HSG should be referred to a tertiary care centre having interventional and Assisted Reproductive Treatment (ART) facility.
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis-Women with unilateral or bilateral proximal tube obstruction confirmed by hysterosalpingography (HSG) or laparoscopy are candidates for fallopian tube recanalization. Proper historical evaluation, general physical and gynaecological examination and exclusion of infective etiology should precede (HSG).
Investigations-
Hysterosalpingography (HSG)
A repeat study may be performed if not performed earlier or earlier study was not satisfactory.
Hysteroscopy or Laparoscopy
Hysteroscopy or laparoscopy can be considered depending on the availability and local expertise in the referred tertiary centre.
Combined Hysteroscopy and Laparoscopy Procedure
Patients with previous history of pelvic inflammatory disease, proximal tubal obstruction may be evaluated by combined hysteroscopy & laparoscopy especially if laparoscopy had not been performed previously. Moreover in patients with uterine mass, hystroscopically guided removal may be preferred over fallopian tube recanalization.
Treatment
Fallopian catheterization
The procedure may be best carried out with use of fluoroscopic guidance if patient has had prior laparoscopy that showed either no or minimal pelvic disease. Small tapered catheters and wires can be easily advanced fluoroscopically if the obstruction is in the isthmic part of the tube, 3-5 cm from the tubal ostium.
Diagnostic Selective Salpingography and Therapeutic fallopian Tube Recanalization
It should be performed in case of non filling of fallopian tubes to differentiate technically inadequate hysterosalpingography or spasm from true obstruction or tubal disorder such as salpingitis isthmica nodosa (SIN).The other indications include discordance between HSG and laparoscopy, prior to recanalization of PTO and persistent hypofertility after surgical tubocornual anastomosis.
Tubal cannulation can be used effectively to restore tubal patency in sub fertility due to isolated PTO, thus helps to avoid expensive assisted reproductive techniques. Tubal cannulation also eliminates or postpone the need for laparoscopic or hysteroscopic interventions by identifying patients with proximal and distal occlusion (bipolar tubal occlusion) and differentiating between true and false diagnoses of PTO.This procedure is reported to be successful in 62%–90% of patients.
Recanalization is possible but potentially less successful in women who have occluded tubes after surgical anastomosis for reversal of tubal ligation. The success rates depend upon postoperative scarring at the anastomosis and range from 44% (12) to 77% (13). In patients with fallopian tube occlusion related to salpingitis isthmica nodosa, recanalization is successful in 77%–82% of tubes (14, 15).
The average pregnancy rates are reported to be about 30% following the procedure (16-19).
Alternative Therapies
Alternative therapies such as microsurgical tubocornual anastomosis, hysteroscopic tube cannulation or falloscopic tube cannulation and in vitro fertilization should be reserved for failed fluoroscopic transcervical fallopian tube recanalization.
Standard Operating procedure
a. In Patient- This is not applicable as fallopian tube recanalization procedure is carried out as day care procedure.
b. Out Patient- Follow up in OPD.
c. Day Care- Fluoroscopic transcervical procedure is carried out as day care procedure.
| Designation | Responsibility |
| Gynaecologist | Clinical Evaluation & diagnostic work up |
| Diagnostic Radiologist | Perform Sonography, HSG , MRI(if required) |
| Gynaecologist trained in laparoscopy & hysteroscopy | Performs laparoscopy or hysteroscopy or both |
| Interventional Radiologist | IR Procedures –Diagnostic selective salpingography and fluoroscopic transcervical fallopian tube recanalization |
| Nursing Staff | Assist in managing the patient |
| Radiographer Technician | Assist in imaging of patient and during interventional procedure |
| Lab Technician (Haematologist & Biochemist) | Haematological & biochemical evaluation |
RESOURCES REQUIRED FOR ONE PATIENT / PROCEDURE (PATIENT WEIGHT 60 KGS)
(Units to be specified for human resources, investigations, drugs and consumables and equipment. Quantity to also be specified)
| SITUATION | HUMAN RESOURCES | INVESTIGATIONS | DRUGS & CONSUMABLES | EQUIPMENT |
| 1. | Doctors – Gynaecologist – 1, Diagnostic Radiologist -1 X ray Technicians –1, Lab technician -1 Nurses - 2 | Hemoglobin, Random Blood Sugar, total & differential blood count, platelet count, ESR , HIV, urine analysis, vaginal smear, chest radiograph, | 1. Drugs: Injection Buscopan, Atropine Diazepam/ Midazolam Doxycycline capsules, Non ionic radiographic contrast, | Color Doppler Ultrasound (1) X ray machine with image intensifier (1) Vaginal speculum, introducer catheter/canula for HSG |
| 2. | Gynaecologist trained in laparoscopy & hysteroscopy-1 Interventional radiologist -1 X ray Technicians – 1 Lab technician -1 Nurses - 2 | Hemoglobin, Random Blood Sugar, total & differential blood count, platelet count, ESR , HIV, urine analysis, vaginal smear, Chest radiograph, | Drugs: Injection Buscopan, Atropine Diazepam/ Midazolam Doxycycline capsules, Recanalization set (Cook) or 5 French and 3 French catheters. 0.018 inch and 0.035 inch hydrophilic guidewire Non ionic radiographic contrast, | Color Doppler Ultrasound (1) X ray machine with image intensifier (1) Vaginal speculum, introducer catheter/ canula for HSG |
Guidelines by The Ministry of Health and Family Welfare :
Dr. Chander Mohan
Dr. B.L. Kapur Hospital New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd