- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Epistaxis - Standard Treatment Guidelines
Epistaxis is bleeding from nose. Blood may flow anteriorly or go posteriorly It may be clotted or flow from nose.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Epistaxis. Following are the major recommendations:
Introduction:
Nose bleeds are common as nose is rich in blood supply and is prominent on the face. Most epistaxis are minor and are managed at home. Only a small percentage comes for medical attention.
Incidence In Our Country
No exact data are available in our country.
Differential Diagnosis
The diagnosis is clinical. Hence it has no differential diagnosis. The various common causes of epistaxis may be local or systemic.
Local causes
1. Low humidity: as in dry climate in summers and winters
2. Infection- Rhinitis, sinusitis
3. Trauma: Injury to nose by direct trauma or by nose picking.
4. Surgery: Septoplasty or endoscopic sinus surgery
Systemic causes:
1. Hypertension
2. Blood thinning drugs like aspirin, clopidogrel, warfarin
3. Benign growths like Angiofibroma and Rhinosporidiosis
4. Cancers like Sinonasal cancers and Carcinoma of nasopharynx
Prevention And Counselling
Epistaxis can be prevented by keeping the nasal mucosa moist in dry climates by douching with water, applying creams and nasal sprays.
Most epistaxis are mild and can be dealt effectively at home. The soft parts of nose are pinched tightly for 10-20 minutes. The head is bent forward and kept above the level of heart. Any blood flowing in to throat should be spit into a bowl. Ice can be applied locally. After the epsitaxis is controlled, patient is advised not to blow nose, keep the nasal mucosa moist and blood pressure under control.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
At Secondary Hospital/ Non Metro Situation
Clinical Diagnosis :
When the epistaxis is not controlled with local pressure for over 20 min, expert medical care is required. The basic evaluation should include:
1. Pulse, BP monitoring,
2. General evaluation of clinical condition
3. Complete ENT examination
4. Nasal examination to identify cause and site of bleeding.
5. Evaluation of extent and site of trauma to face if any
Investigations :
1. complete blood count,
2. bleeding and clotting time.
3. X Ray of paranasal sinuses and nasal bones in trauma.
4. Other investigations based on general clinical condition
Treatment :
Out Patient : General condition of the patient is stabilized.
Day Care :
1. If the site of bleeding is identified, chemical or electro cautery is done to stop the bleeding.
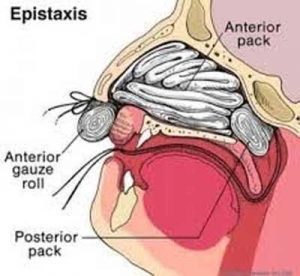
2. If not, then anterior nasal packing is done with ribbon gauze soaked in liquid paraffin and antibiotic solution, gelfoam or hemostatic sponge. The packs are kept in place for two to three days.
Inpatient :
1. It the bleeding still continues, a posterior nasal packing with gauze or Foley’s catheter may be done.
2. Manangement of comorbities.
Referral Criteria :
1. Massive blood loss
2. Bleeding not controlled with anterior and posterior nasal packing.
3. Midface fractures would require a maxillofacial consultation.
4. Other co morbidities requiring appropriate cross consultations.
At Tertiary Hospital/ Metro Situation
Clinical Diagnosis :
When the epistaxis is not controlled with anterior and posterior nasal packing, the evaluation should include:
1. Review of general evaluation of clinical condition
2. Complete ENT examination
3. Nasal Endoscopic examination under Local/ General Anaesthesia to identify cause and site of bleeding.
4. Evaluation of extent and site of trauma to face if any
Investigations :
1. complete blood count,
2. bleeding and clotting time.
3. Prothrombin Time/ PTTK/ INR
4. Contrast enhanced CT Scan of paranasal sinuses
5. MR Angiography
6. Digital substraction angiography (DSA) of carotid and vertebral artery system
Treatment :
Additional measures which may be required are
Out Patient / Day Care : Endoscopic electro cautery
Inpatient :
1. Septoplasty
2. Maxillofacial reduction of fracture and wire and plate fixation.
3. External carotid artery ligation
4. DSA embolisation of bleeding vessel
5. Biopsy and / or excision of tumor if any
6. Management of comorbidiites.
Referral Criteria :
1. In adequate facilities for any of the above.
Guidelines by The Ministry of Health and Family Welfare :
Dr J M Hans Ex-HOD Dept. of Otorhinolaryngology Dr.RML Hospital New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd