- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Eliminating opioids from anesthesia decreases post-operative nausea
Opioid-free general anesthesia is safe, effective and dramatically decreases postoperative nausea, according to a single-center study of more than 1,000 patients being presented at the ANESTHESIOLOGY® 2017 annual meeting.
Using opioid alternatives during general anesthesia is part of an effort by TEAMHealth Anesthesia at Select Physicians Surgery Center in Tampa, Florida to reduce the use of opioids during and after surgery. The study findings suggest physician anesthesiologists are helping pave the way to promote pain management alternatives to opioids, and making headway in reducing the use of the addictive medications.
"Opioids crept into general anesthesia over the years because they don't cause problems with the cardiovascular system, but our research suggests we can use alternatives safely and effectively," said David Samuels, M.D., lead author of the study and medical director of anesthesia at Select Physicians Surgery Center and medical director for TEAMHealth Anesthesia, Tampa. "By avoiding the use of opioids intraoperatively and helping surgeons understand the value and importance of offering patients different options for pain after surgery, physician anesthesiologists can be agents of change in addressing the opioid dependency crisis."
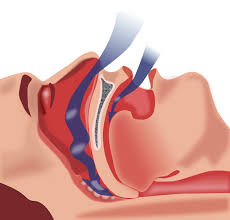
Opioids - usually fentanyl, an opioid 50 times more powerful than heroin - are typically included in the combination of medications given to patients for general anesthesia during surgery. In the study, 1,009 patients having head and neck surgery (including laryngoscopy, complex facial plastic surgery, middle ear surgery and nasal or sinus surgery) received general anesthesia without opioids. Instead, patients received various combinations of magnesium, sub-anesthetic ketamine, lidocaine and ketorolac, depending on the patient's age and health. Surgeons and patients expressed a high degree of satisfaction with the new anesthesia protocol and postoperative pain management.
After surgery, 11 percent of patients experienced nausea, whereas 50 to 80 percent of patients typically suffer from nausea after surgery. Additionally, 64 percent of patients did not require any pain medication in the PACU.
The traditional use of fentanyl in general anesthesia can cause hyperalgesia, or increased sensitivity to pain, Dr. Samuels said.
"Hyperalgesia leads to increased pain, so patients request more opioids in the recovery area, and then go home with an excessive number of pills," said Enrico M. Camporesi, M.D., co-author of the study and professor emeritus at the University of South Florida and director of research for TEAMHealth Anesthesia Research Institute, Tampa. "We believe that not using fentanyl during surgical anesthesia, as well as not providing patients too many pills after surgery, may help decrease the likelihood of opioid abuse. Studies show that 1 in 15 patients who has surgery is still taking prescription opioids 90 days afterwards," he said.
Three of the 19 surgeons who participated in the study now prescribe patients daily oral magnesium, gabapentin and ibuprofen for pain management after surgery. They also prescribe five hydrocodone pills for any breakthrough pain. Previously, these surgeons prescribed 50 hydrocodone pills. The change to five pills will lead to 27,000 fewer prescribed hydrocodone pills in one year's time for these surgeons at their practice.
The researchers say they plan to study whether avoiding opioids during surgery and reducing opioid prescriptions after surgery leads to reduced opioid use and abuse.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd