- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
EDF Management Guidelines for Anogenital Warts
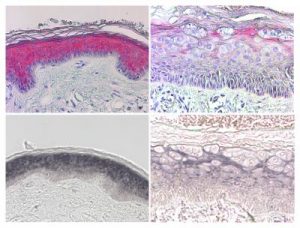
In order to update previously published European guidelines for the management of anogenital warts, Dr.Charles Lacey and associates performed a systematic review of randomized controlled trials for anogenital warts.They analyzed and collated the same as Guideline.They include Recommendations for Diagnosis, Home Therapy, Office therapy, Vaginal, cervical, intra-meatal, intra-anal warts and treatment in pregnancy and immunocompromised patients.The Guidelines have been published in Journal of the European Academy of Dermatology and Venereology.
Recommendations for Diagnosis:
- Examine with a good light; a lens or colposcope may be useful for small lesions.
- In men, always examine the meatus, and have a low threshold for examining the perianal area and performing proctoscopy to examine the anal canal. In women, always examine the perianal area and perform a speculum examination to exclude cervical or vaginal lesions, and have a low threshold for performing proctoscopy to examine the anal canal. Proctoscopy is safe in subjects with perianal warts.
- Biopsy is not necessary for typical anogenital warts; biopsy must always be performed if there is any suspicion of precancer or cancer, and can be useful for differential diagnosis
- Not all papular lesions are caused by HPV. Always consider normal variants such as pearly penile papules and Fordyce spots and differential diagnoses such as molluscum contagiosum, seborrheic keratoses, etc.
- HPV typing of anogenital warts does not add information of clinical use, and is not recommended
- Some practitioners use the acetic acid test to diagnose subclinical HPV lesions; its place in diagnosis and management remains controversial.
Recommendations for Home Therapy
- Podophyllotoxin 0.5% solution and 0.15% cream:
- Each course of podophyllotoxin treatment comprises self application twice daily for 3 days, followed by four rest days. Use of 0.5% podophyllotoxin solution is convenient for penile warts. However, vulvar and anal warts are more feasibly and efficiently treated with 0.15% podophyllotoxin cream, when inspection, often aided by a mirror and digital palpation, facilitate the application procedure
- Podophyllotoxin is contraindicated during pregnancy, and women of childbearing age must use contraception or abstain from penetrative sexual activity during therapy.
- Imiquimod cream 5% (Ib, A):
- Imiquimod cream is supplied as a package of twelve single use sachets. It is applied to the warts three times a week at bedtime and the area washed with soap and water the next morning. Treatment continues until wart clearance, or for a maximum of 16 weeks. Local reactions at the treatment site may occur and these can be managed by a rest period of several days, or by reducing the frequency of application.
- Erythema is often seen as a side effect with imiquimod therapy, and sometimes appears to precede clinical resolution. Occasionally severe inflammation is seen necessitating discontinuation of therapy. Phimosis and lichen sclerosis after therapy have also been reported.
- More data is needed before imiquimod cream can be considered safe during pregnancy.
- Sinecatechins (Veregen 10% ointment) (Ib, A)(available in the United States, Germany and Austria.):
- The ointment is applied three times a day until complete clearance, or for up to 16 weeks.
- It cannot be used internally or in pregnancy.
- Cryotherapy (Ib, A):
- Cryotherapy can be delivered by ‘open’ (liquid nitrogen) or ‘closed’ systems.
- Open application of liquid nitrogen is usually delivered by spray gun device, freezing the lesion and a margin of healthy skin for about 20 s.
- Closed cryoprobe systems utilize circulation of nitrous oxide or carbon dioxide, the probe gently pressed to the surface moistened with saline or lubricating jelly and freezing performed until a freezing ‘halo’ occurs a few millimetres around the lesion. A freeze-thaw-freeze technique is applied to each lesion at each session. Application techniques are difficult to standardize and there may be significant intra-operator differences.
- Cryotherapy is usually performed at weekly intervals, although no studies have systematically evaluated different treatment intervals.
- Trichloracetic acid (TCA) 80–90% solution (Ib, A):
- It is applied sparingly directly to the wart surface with either the wooden or a cotton tip end of an applicator, as per preference, and is usually applied weekly.
- It is most suitable for small acuminate or papular warts but less easy to use on keratinized or large lesions.
- TCA is corrosive and overzealous use may cause scarring. A neutralising agent (for example, sodium bicarbonate) should be readily available in case of excess application or spills.
- When used optimally, a shallow ulcer forms that heals without scarring.
- TCA can be used safely during pregnancy.
- Surgical treatment:
- A variety of surgical techniques are in use, including electrosurgery, curettage, scissors excision and laser therapy.
- Surgery may be used as primary therapy, and the majority of patients can be treated under local anaesthesia.
- Routine use of local anaesthetic cream is recommended before infiltration anaesthesia, reducing discomfort from injections significantly. Use of up to 100 mg lidocaine, as 5 mL of 2% or 10 mL of 1%, for infiltration gives rapid anaesthesia of the epithelium.
- Adrenaline as adjuvant reduces bleeding but is contraindicated on the penis and in the clitoris region, and clinics therefore may choose not to stock the combined preparations to prevent inadvertent inappropriate use.
- Electrosurgery (Ib, A) scissors excision (Ib, A), curettage and laser surgery (IIa, B):
- Modern electrosurgical units utilize alternating current to produce different types of wave forms resulting in blends of cutting and coagulation. These systems use isolated circuitry, can be monopolar or bipolar, and vary from small simple devices to larger complex systems.
- Scissors excision is useful when smaller numbers of lesions are present and may be assisted by diathermy to control bleeding and to destroy any conspicuous wart tissue remaining after the excision.
- Curettage is a simple effective technique for small numbers of lesions, and either diathermy or silver nitrate is used for haemostasis.
- Carbon dioxide and YAG laser emissions result in very high power densities being delivered to small tissue volumes.
- Both electrosurgery and laser surgery should be performed with the use of surgical masks by the treatment team, and the use of a smoke evacuator
- Formal surgery (IVc) – bulky warts, extensive warts, anal ⁄ intra-anal warts and significant lesions in children are most conveniently removed under general anaesthesia by an appropriate surgical specialist.
- Vaginal warts can be treated with either TCA or cryotherapy.
- Cervical warts should be managed by a gynaecologist. Intra-meatal warts can be treated with either TCA or various surgical techniques.
- TCA can be used for small volume intra-anal warts, and imiquimod use is feasible with suitable patient motivation.
- Otherwise formal surgical referral is indicated for intra-anal warts
- In pregnancy warts may enlarge and multiply. Genital warts present at delivery are associated with a risk of approximately 1 in 400 of the infant developing juvenile laryngeal papillomatosis.
- There is no proof that treatment diminishes this risk, although reduction of viral burden would seem wise.
- Liason with the obstetrician in management is recommended.
- Spontaneous regression of genital warts is very frequently seen in the puerperium.
- Both HIV infection and iatrogenic immunosuppression are associated with an increased prevalence of anogenital warts.
- the response to treatment in HIV positive subjects is impaired, and recurrences after treatment are more common.Recent studies of the use of imiquimod in patients treated with HAART showed total clearance rates of 31–32%, whereas an RCT of surgery combined with imiquimod demonstrated a 100% primary clearance.
- Condom use is recommended within partnerships when either subject has genital warts until resolution of lesions (lb; A)
- Current partners and, if possible, other partners within the past 6 months, should be assessed for the presence of lesions and for education and counselling about STDs and their prevention.
- It is good practice for units treating patients with genital warts to develop their own treatment algorithms including local practice and recommendations.
- Such patient level management protocols should incorporate medical review of cases at least every 4 weeks, with switching of treatments if an inadequate response is observed.
Physicians treating patients with genital warts should develop their own treatment algorithms which include local practice and recommendations. Such patient level management protocols should incorporate medicalreview of cases at least every 4 weeks, with switching of treatments if an inadequate response is observed. First episode patients should be offered sexually transmitted disease screening. Management should include partner notification and health promotion.
To Read the full guideline click on the following link :

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd