- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
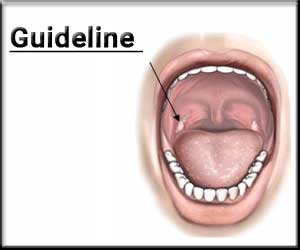
Do Not Prescribe Perioperative Antibiotics for tonsillectomy in Children: New ENT Guideline
Clinicians should not administer or prescribe perioperative antibiotics to children undergoing tonsillectomy is an important recommendation put forward by the recently issued guideline update provided by the American Academy of Otolaryngology-Head and Neck Surgery. The guideline update also strongly recommended against administering or prescribing codeine, or any medication containing codeine, after tonsillectomy in children younger than 12 years.
The American Academy of Otolaryngology-Head and Neck Surgery Foundation published the Clinical Practice Guideline: Tonsillectomy in Children (Update) today in Otolaryngology-Head and Neck Surgery. The update to the 2011 publication, which includes a large amount of new information that applies to a child considered for tonsillectomy, emphasizes education, counseling, and pain management with several tables and handouts that are user-friendly and helpful to caregivers.
"The purpose of this multidisciplinary guideline is to identify quality improvement opportunities in managing children, 18 years of age or less, who are under consideration for tonsillectomy and to create explicit and actionable recommendations. The goal is to educate clinicians and caregivers on the indications and the perioperative management of children undergoing tonsillectomy. There is an emphasis on the need for evaluation and intervention in special populations. We highlight the need for counseling and education of families," said Ron B. Mitchell, MD, Chair of the guideline update group.
Tonsillectomy is a surgical procedure performed with or without adenoidectomy that completely removes the tonsil, including its capsule, by dissecting the peritonsillar space between the tonsil capsule and the muscular wall. Tonsillectomy is one of the most common ambulatory surgery procedures performed on children in the U.S.
Changes in practice since the 2011 guideline include a reduction in the use of routine postoperative antibiotics as well as a Food and Drug Administration black box warning on the use of codeine in children posttonsillectomy.
"The frequency of performing tonsillectomy in children, coupled with the significant practice variations in diagnosing and managing children undergoing the surgery, supported the need for an updated evidence-based clinical practice guideline to replace the 2011 version," said Dr. Mitchell.
Changes from the prior guideline include two consumer advocates added to the update group; evidence from one new clinical practice guideline, 26 new systematic reviews, and 13 new randomized controlled trials; enhanced emphasis on patient education and shared decision-making; the addition of an algorithm to clarify action statement relationships; changes to five of the key action statements (KASs) from the original guideline; incorporation of new evidence profiles to include the role of patient preferences, confidence in the evidence, differences of opinion, quality improvement opportunities, and any exclusion to which the action statement does not apply; and the addition of seven new KASs.
Following are the important DOs and DONT recommendations in the form of key action statements put forward by the guideline update
DOs
The guideline update group made strong recommendations for the following key action statements (KASs):
(1) Clinicians should recommend watchful waiting for recurrent throat infection if there have been <7 episodes in the past year, <5 episodes per year in the past 2 years, or <3 episodes per year in the past 3 years.
(2) Clinicians should administer a single intraoperative dose of intravenous dexamethasone to children undergoing tonsillectomy.
(3) Clinicians should recommend ibuprofen, acetaminophen, or both for pain control after tonsillectomy.
The guideline update group made recommendations for the following KASs:
(1) Clinicians should assess the child with recurrent throat infection who does not meet criteria in KAS 2 for modifying factors that may nonetheless favor tonsillectomy, which may include but are not limited to multiple antibiotic allergies/intolerance, PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and adenitis), or history of >1 peritonsillar abscess.
(2) Clinicians should ask caregivers of children with obstructive sleep-disordered breathing and tonsillar hypertrophy about comorbid conditions that may improve after tonsillectomy, including growth retardation, poor school performance, enuresis, asthma, and behavioral problems.
(3) Before performing tonsillectomy, the clinician should refer children with obstructive sleep-disordered breathing for polysomnography if they are <2 years of age or if they exhibit any of the following: obesity, Down syndrome, craniofacial abnormalities, neuromuscular disorders, sickle cell disease, or mucopolysaccharidoses.
(4) The clinician should advocate for polysomnography prior to tonsillectomy for obstructive sleep-disordered breathing in children without any of the comorbidities listed in KAS 5 for whom the need for tonsillectomy is uncertain or when there is discordance between the physical examination and the reported severity of obstructive sleep-disordered breathing. (
5) Clinicians should recommend tonsillectomy for children with obstructive sleep apnea documented by overnight polysomnography.
(6) Clinicians should counsel patients and caregivers and explain that obstructive sleep-disordered breathing may persist or recur after tonsillectomy and may require further management.
(7) The clinician should counsel patients and caregivers regarding the importance of managing posttonsillectomy pain as part of the perioperative education process and should reinforce this counseling at the time of surgery with reminders about the need to anticipate, reassess, and adequately treat pain after surgery.
(8) Clinicians should arrange for overnight, inpatient monitoring of children after tonsillectomy if they are <3 years old or have severe obstructive sleep apnea (apnea-hypopnea index ≥10 obstructive events/hour, oxygen saturation nadir <80%, or both).
(9) Clinicians should follow up with patients and/or caregivers after tonsillectomy and document in the medical record the presence or absence of bleeding within 24 hours of surgery (primary bleeding) and bleeding occurring later than 24 hours after surgery (secondary bleeding).
(10) Clinicians should determine their rate of primary and secondary posttonsillectomy bleeding at least annually.
DONT's
The guideline update group made a strong recommendation against 2 actions:
(1) Clinicians should not administer or prescribe perioperative antibiotics to children undergoing tonsillectomy.
(2) Clinicians must not administer or prescribe codeine, or any medication containing codeine, after tonsillectomy in children younger than 12 years.
The policy level for the recommendation about documenting recurrent throat infection was an option:
(1) Clinicians may recommend tonsillectomy for recurrent throat infection with a frequency of at least 7 episodes in the past year, at least 5 episodes per year for 2 years, or at least 3 episodes per year for 3 years with documentation in the medical record for each episode of sore throat and ≥1 of the following: temperature >38.3°C (101°F), cervical adenopathy, tonsillar exudate, or positive test for group A beta-hemolytic streptococcus.
To read the guideline in detail, click on the following link
Ron B. Mitchell, Sanford M. Archer, Stacey L. Ishman, Richard M. Rosenfeld, Sarah Coles, Sandra A. Finestone, Norman R. Friedman, Terri Giordano, Douglas M. Hildrew, Tae W. Kim, Robin M. Lloyd, Sanjay R. Parikh, Stanford T. Shulman, David L. Walner, Sandra A. Walsh, Lorraine C. Nnacheta. Clinical Practice Guideline: Tonsillectomy in Children (Update). Otolaryngology–Head and Neck Surgery, 2019; 160 (1_suppl): S1 DOI: 10.1177/0194599818801757

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd