- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Direct‐Acting Antiviral Therapy Cuts Liver Cancer Risk By 71%
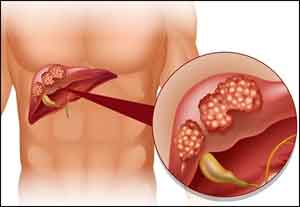
A new study presented this week at The Liver Meeting — held by the American Association for the Study of Liver Diseases — found that eradication of the hepatitis C virus-induced by direct‐acting antiviral medications is associated with a 71 percent reduction in the risk of liver cancer.
Hepatitis C virus, commonly called HCV, is one of the several viruses that can infect the liver. According to the Centers for Disease Control and Prevention, approximately 2.7 million people in the United States are infected with HCV. And, HCV along with chronic hepatitis B virus infections account for approximately 78 percent of all liver cancer cases worldwide.
Researchers at the University of Washington, Seattle and the Veterans Affairs Puget Sound Healthcare System in Seattle recently conducted a study to determine whether the eradication of HCV with direct-acting antivirals — used to stop the lifecycle of HCV — could reduce liver cancer risk in patients.
To date, it has been unclear whether eradicating HCV through DAA treatment (referred to as sustained virological response) reduced the risk of liver cancer in patients infected with HCV. The researchers of this study also sought to compare the response to DAA regimens and interferon‐based regimens. The researchers repeated and extended their analysis to June 2017 in order to identify more incident cancers, especially in the DAA‐only treatment group.
“The majority of primary liver cancers in the United States occur in patients with hepatitis C virus infection. It is tempting to assume that if we eradicate hepatitis C, the risk of liver cancer will also be eradicated or at least substantially reduced,” says George N. Ioannou, MD, MS, associate professor of gastroenterology at the University of Washington School of Medicine, and lead investigator in the study.
“However, patients with hepatitis C may already have developed cirrhosis or advanced fibrosis before the hepatitis C is eradicated, which may put them at risk of liver cancer even after hepatitis C is eradicated. Furthermore, recent studies suggested an increased risk of liver cancer in patients with HCV who were treated with the new DAAs. This made it all the more imperative for us to determine whether DAA‐induced eradication of HCV is associated with a reduction in liver cancer risk using an adequately powered study,” he says.
The researchers identified 62,051 patients who underwent 83,695 antiviral treatment regimens in the VA Puget Sound Healthcare System from 1999 to 2015. The data included 35,873 interferon‐only regimens, 26,178 DAA±interferon regimens and 21,644 DAA‐only regimens. They used Cox proportional hazards regression to determine the association between HCV eradication and liver cancer risk after adjusting for a large number of potential confounders.
Dr. Ioannou’s team identified 3,271 incident cases of liver cancer diagnosed at least 180 days after initiation of antiviral treatment during an average follow‐up of 6.1 years. The incidence of liver cancer was highest in patients with cirrhosis and treatment failure (3.25 per 100 patient‐years), followed by cirrhosis and sustained virological response (1.97), no cirrhosis and treatment failure (0.87) and no cirrhosis and sustained virological response (0.24). Sustained virological response was associated with a significantly decreased risk of liver cancer in multivariable models regardless of whether the antiviral treatment was DAA‐only (adjusted hazard ratio [AHR] 0.29, 95% CI 0.23‐0.37), DAA+interferon (AHR 0.48, 95% CI 0.32‐0.73) or interferon‐only (AHR 0.32, 95% CI 0.28‐0.37). Receipt of a DAA‐only or DAA+interferon regimen was not associated with increased HCC risk compared to receipt of an interferon‐only regimen.
The study’s findings showed that DAA‐induced sustained virological response is associated with a 71 percent reduction in patients’ liver cancer risk, and showed treatment with DAAs is not associated with increased liver cancer risk compared to treatment with interferon.
“Eradicating hepatitis C will have a tremendous benefit in reducing liver cancer in individual patients and in the entire population,” says Dr. Ioannou. “Physicians and patients should not be withholding antiviral treatment for fear of inducing liver cancer. On the contrary, physicians should be treating hepatitis C specifically to reduce the risk of liver cancer.”

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd