- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Dengue fever in children - Standard Treatment Guidelines

Dengue has a wide spectrum of clinical presentations, often with unpredictable clinical evolution and outcome. Reported case fatality rates are approximately 1%, but in India, Indonesia and Myanmar, focal outbreaks away from the urban areas have reported casefatality rates of 3-5%.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Protocol for dengue fever in children. Following are the major recommendations :
Classification and Case definition
The Newer WHO Classification of Dengue is practical from the management perspective and involves 2 categories- Dengue and Severe Dengue [including both the previously classified categories Dengue Shock Syndrome and Dengue Haemorrhagic
fever]
Case definition of Dengue fever (DF) :
Dengue fever is an acute febrile illness with one or more of the following:- Headache, retrorbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, and leukopenia and lab confirmation by ELISA.
Case Definition of Severe Dengue
Severe dengue should be considered if the patient is from an area of dengue risk presenting with fever of 2–7 days plus any of the following features:
- There is evidence of plasma leakage, such as:
- high or progressively rising haematocrit;
- pleural effusions or ascites;
- circulatory compromise or shock (tachycardia, cold and clammy extremities, capillary refill time greater than three seconds, weak or undetectable pulse, narrow pulse pressure or, in late shock, unrecordable blood pressure).
- There is significant bleeding.
- There is an altered level of consciousness (lethargy or restlessness, coma, convulsions).
- There is severe gastrointestinal involvement (persistent vomiting, increasing or intense abdominal pain, jaundice).
- There is severe organ impairment (acute liver failure, acute renal failure, encephalopathy or encephalitis, ARDS or other unusual manifestations. )
Warning Signs in Dengue Fever
- Abdominal pain or tenderness
- Persistent vomiting
- Clinical fluid accumulation
- Mucosal bleed
- Lethargy, restlessness
- Liver enlargement >2 cm
- Laboratory: increase in HCT concurrent with rapid decrease in platelet count *(requiring strict observation and medical intervention)
Differential diagnosis
Conditions that mimic the febrile phase of dengue infection
- Influenza,
- Measles,
- Chikungunya,
- Infectious
- Mononucleosis,
- HIV Seroconversion Illness
- Rubella,
- Scarlet Fever,
- Meningococcal infection,
- Drug reaction
- Enteric infections
- Meningo/encephalitis
- Febrile seizures
Conditions that mimic the critical phase of dengue infection
- Acute gastroenteritis,
- Malaria,
- Leptospirosis,
- Typhoid,
- Typhus,
- Viral hepatitis,
- Acute HIV, seroconversion illness,
- Bacterial sepsis, septic shock
- Malignancies Acute leukaemia and other malignancies
Investigations
Situation 1
Diagnostic Methods
| Test | Advantage | Disadvantage |
| Antigen Detection [NS-1] | · Easy to perform · Early detection | · Not as sensitive as above |
| IgM assay | · Less expensive · Easy to perform · Useful in outbreaks | · May miss secondary infection due to undetectable IgM · Useful only after 5 days · Cross reactivity |
Supportive Tests
- Complete Blood Count-Hemoglobin, haematocrit, White Cell Count, Platelet count.
- Blood grouping and Cross Matching.
- Peripheral smear: Indicates the type of anemia and confirms leukopenia
The presence of giant platelets and clumps is indicative of good platelet function - Serum electrolytes, Urea, Creatinine, Random Blood Sugar
- Liver and renal function tests.
- Chest X Ray
Treatment
Situation 1
Out Patient Management
Simple Dengue Fever with no warning signs, adequate oral intake and clinically
well.
Home Care Advice
- Adequate rest
- Adequate fluid intake - Milk, fruit juice, electrolyte solution (ORS) and barley/rice water.
- Paracetamol [ Acetylsalicylic acid, Mefenemic acid, ibuprofen or other nonsteroidal anti-inflammatory agents (NSAIDs) and steroids to be avoided.]
- Tepid sponging
- To look for mosquito breeding places in and around the home and eliminate them
- Antibiotics are not necessary.
To observe for the following Danger signs and report immediately for hospital admission
- Bleeding:
- red spots or patches on the skin
- bleeding from nose or gums
- vomiting blood
- black-coloured stools
- heavy menstruation/vaginal bleeding
- Frequent vomiting
- Severe abdominal pain
- Drowsiness, mental confusion or seizures
- Pale, cold or clammy hands and feet
- Difficulty in breathing
Out -patient laboratory monitoring- as indicated
- Haematocrit
- White cell count
- Platelet count
Admission Criteria to Secondary Centre
- Child having high fever, poor oral intake, or any danger signs as enumerated above.
- If platelet count < 100,000 /cu.mm or rapidly decreasing trend.
- If haematocrit is rising trend.
- Special Social Circumstances (living far from a health facility without reliable means of transport).
Admission Criteria to Tertiary Centre directly from OPD
- If signs of severe dengue or warning signs.
- If < 50,000/cu.mm to refer to Tertiary facility
- If Dengue fever is present with other co-morbidities
Management
- Encourage oral fluids. If not tolerated, start intravenous isotonic fluid therapy with or without dextrose at maintenance. Give only isotonic solutions.[ see annexure 1] Start with 5 ml/kg/hour for 1–2 hours, then reduce by 2ml/kg/hour every 2 hours till 2ml/kg/hr provided there is clinical improvement and haematocrit is appropriately improving. IV fluids are usually required for 1-2 days.
- Reassess the clinical status and repeat the haematocrit after 2 hours. If the haematocrit remains the same, continue with the same rate for another 2–4 hours and reassess. If the vital signs/haematocrit is worsening increase the fluid rate and refer immediately.
- Switch to oral as soon as tolerated, total fluid therapy usually 24-48 hrs, titrated to adequate urine output.
Tests for Monitoring:
- Frequent recording of vital signs and investigation are essential for evaluating the results of treatment.
- Temperature, Pulse, blood pressure and respiration should be recorded every hour (or more often) until stable subsequently 2 hourly.
- An hourly fluid balance sheet should be kept, recording the type of fluid and the rate and volume of its administration in order to evaluate the adequacy of fluid replacement.
- Chest X-ray, ultrasound abdomen, electrolytes 12-24 hrly as when clinically indicated
Referral Criteria
- All patients with Warning signs and signs of Severe dengue.
- Patients not clinically responding to therapy in situation.
- Patients with serious co-morbid conditions
- Platelet counts < 50,000/cu.mm with a decreasing trend.
Situation 2
Diagnostic Tests
As in situation 1 in addition the following tests may be useful -
| Test | Advantage | Disadvantage |
| PCR | · Sensitive · Rapid turn around | · Expensive |
| IgM/IgG ratio | · Can differentiate between primariy and secondary dengue | · No standardisation |
Supportive Tests
As in Situation1 and in addition-
- Blood gases.
- Coagulation studies
- Ultrasound
- CT scan
- ECHO
Admission Criteria
Same as in Situation 1 in addition
All patients fulfilling referral criteria form secondary care centres presenting directly or referred.
Pre requisites for management
• Paediatric Intensive care facilities should be available.
Management:
- Obtain a reference haematocrit before fluid therapy. Give only isotonic solutions. Start with 5–7 ml/kg/hour for 1–2 hours, then reduce to 3–5 ml/kg/hr for 2–4 hours, and then reduce to 2–3 ml/kg/hr or less according to the clinical response.
- Reassess the clinical status and repeat the haematocrit. If the haematocrit remains the same or rises only minimally, continue with the same rate (2–3 ml/kg/hr) for another 2–4 hours. If the vital signs are worsening and haematocrit is rising rapidly, increase the rate to 5–10 ml/kg/hour for 1–2 hours. Reassess the clinical status, repeat the haematocrit and review fluid infusion rates accordingly.
- Give the minimum intravenous fluid volume required to maintain good perfusion and urine output of about 0.5 ml/kg/hr. Intravenous fluids are usually needed for only 24–48 hours. Reduce intravenous fluids gradually when the rate of plasma leakage decreases towards the end of the critical phase. This is indicated by urine output and/or oral fluid intake that is/are adequate, or haematocrit decreasing below the baseline value in a stable
patient. - Patients with warning signs should be monitored by health care providers until the period of risk is over.
- Supportive Management- antipyretics, empirical antibiotics as clinically indicated.
Monitoring as follows-
- A detailed fluid balance should be maintained. Parameters that should be monitored include hourly vital signs and peripheral perfusion. (Until the patient is out of the critical phase), urine output (hourly).
- Arterial blood pressure monitoring and central venous pressure monitoring ideal for all children in shock who are fluid unresponsive. Arterial blood gas monitoring as clinically indicated. Infusion pump will help in precise regulation of fluid input.
- Haematocrit (before and after fluid replacement/change, Hourly to 2nd hourly haematocrit for first 6 hours , decreasing frequency as patient improves ), Platelet counts 12 hourly blood glucose, and other organ functions (such as renal profile, liver profile, coagulation profile, as indicated).
- Chest x-ray –Effusions, pulmonary edema
- Echocardiogram for assessment of left ventricular function, dimensions and
- regional wall dyskinesia
- ECG to exclude arrhythmia;
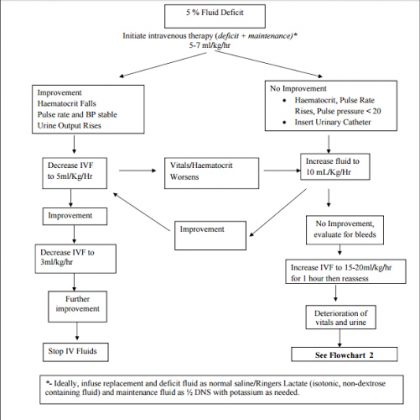
Treatment of Shock- See flow chart 1
Treatment of haemorrhagic complications
- A drop in haematocrit with no clinical improvement despite adequate fluid administration indicates significant internal bleeding. Internal bleeding is difficult to recognize in the presence of haemo-concentration. First correct the component of shock according to standard guidelines with early use of packed cell transfusion. Component transfusion is indicated in cases with significant clinical bleeding.
- The results of hematological tests (PT, APTT) may be studied to document the severity of DIC Transfusion of cryoprecipitate and or fresh frozen plasma should be considered in cases of DIC with bleeds.
- Indications for platelet transfusion
- Shock, acidosis with rapidly declining platelets ( greatest risk of DIC)
- Significant mucosal bleeds (harbinger of intracranial hemorrhage)
- Platelet count < 20,000 cu mm in the acute phase
- Need for invasive procedures such as central lines maintain platelet count > 50,000 cu mm
- A low platelet count is less significant after recovery from shock and may not need to be transfused.
Treatment of Fluid overload
Fluid overload with large pleural effusions and ascites is a common cause of acute respiratory distress and failure in severe dengue. Other causes of respiratory distress include acute pulmonary oedema, severe metabolic acidosis from severe shock, and Acute Respiratory Distress Syndrome (ARDS)
Prevention of fluid overload
- When the following signs are present, resuscitation intravenous fluids should be discontinued or reduced to the minimum rate necessary to maintain euglycaemia:
- signs of cessation of plasma leakage;
- stable blood pressure, pulse and peripheral perfusion;
- haematocrit decreases in the presence of a good pulse volume;
- afebrile for more than 24–48 days (without the use of antipyretics);
- resolving bowel/abdominal symptoms;
- improving urine output.
- Aim for a minimum acceptable urine output [ 0.5ml/kg/hr] to titrate fluids.
- Maintain intravascular volume by using colloids and maintaining oncotic pressure.
The action plan for the treatment of fluid overload is as follows:
- Oxygen therapy/ventilation if indicated should be given immediately.
- Stopping intravenous fluid therapy during the recovery phase will allow fluid in the pleural and peritoneal cavities to return to the intravascular compartment resulting ion dieresis.
- Diuretics as given below
If the patient has stable haemodynamic status and is out of the critical phase (more than 24–48 hours of defervescence)
- Stop intravenous fluids but continue close monitoring.
- If necessary, give oral or intravenous furosemide 0.1–0.5 mg/kg/dose once or twice daily, or a continuous infusion of furosemide 0.1 mg/kg/hour. Monitor serum potassium and correct the ensuing hypokalaemia.
If the patient has stable haemodynamic status but is still within the critical phase, reduce the intravenous fluid accordingly.
- Avoid diuretics during the plasma leakage phase.
- Patients who remain in shock with low or normal haematocrit levels but show signs of fluid overload may have occult haemorrhage. Further infusion of large volumes of intravenous fluids will lead only to a poor outcome. If the patient remains in shock and the haematocrit is elevated, repeated small boluses of a colloid solution may help.
Other Complications of Dengue
- Hypo/Hyperglycemia
- Electrolyte abnormalities
- Nosocomial/Co-infection
- Metabolic Acidosis
Should be managed under standard ICU protocols
Supportive Care and Adjuvant Therapy
This may include:
- Renal replacement therapy, with a preference to continuous veno-venous haemodialysis (CVVH), or peritoneal dialysis if the former unavailable;
- Vasopressor and inotropic therapies as temporary measures to prevent lifethreatening hypotension in dengue shock and during induction for intubation, while correction of intravascular volume is being vigorously carried out;
- Further treatment of organ impairment, such as severe hepatic involvement or encephalopathy or encephalitis; cardiac abnormalities, such as conduction abnormalities, may occur.
Criteria for discharge:
- Absence of fever for at least 24 hrs.
- Return of appetite.
- Clinical improvement.
- Good urine output.
- Stable haematocrit.
- 2 days after recovery from shock.
- No respiratory distress from pleural effusion and ascitis.
Annexure
Immediate replacement of plasma loss/ Issotonic solutions: (1,2)
This should be done with any of the following solutions;
- Normal saline.
- Ringer’s lactate
- In severe/refractory shock, colloids such as Plasma , plasma substitutes (6% hetastarch/dextran/ / 5% albumin /) may be preferred
- Fresh whole blood or packed red blood cells may be needed for persistent shock despite restoration of fluid volume and a fall in haematocrit, suggesting the possibility of occult blood loss.
- Rapidly administered dextrose containing solution when used for resuscitation may result in hyperglycemia and osmotic diuresis, delaying correction of hypovolaemia. Secondly, dextrose is rapidly metabolized resulting in a hypotonic solution that is inappropriate for shock correction.
Recognition of Shock
The following clinical signs should indicate the presence of shock
Tachycardia , Low pulse volume
Capillary Refill time > 2 sec
Narrow pulse pressure
Blood pressure less than the 3rd centile for age
Cold clammy peripheries
Altered sensorium
Poor urine output [ <0.5ml/kg/hr consistently ]
Tachypnoea
Metabolic acidosis
Choice of Vasoactive agents/ post resuscitation fluid removal (8)
- Shock with low BP for age: Dopamine 10mcg/kg/min OR Noradrenaline /adrenaline 0.1-0.2mcg/kg/min
- Shock with normal BP for age: Dobutamine 5-10mcg/kg/min
- Shock with diastolic dysfunction on echo: Milrinone 0.25-0.75mcg/kg/min (no loading dose) Predominant pulmonary edema, haemodynamics stable : Nitroglycerine 1- 3mcg/kg/min, furosemide infusion 3- 5mg/kg/day, titrate to urine output of 3-5 ml/kg/hr. Cease infusion and infuse fluid if hypoperfusion occurs.
- Pulmonary edema, fluid overload, haemodynamics unstable: Ventilation vital (high risk of mortality), can consider peritoneal dialysis if 24 hour experienced nursing and medical staff available in PICU
Good Clinical Practice
- Serial haematocrit measurement (if not bleeding), and urine output provide the most objective guides to fluid replacement and prevention of fluid overload.
- In shock –fluid resuscitate with 10-20ml/Kg of isotonic fluids over 30-60 minutes. Consider in severe shock
- Aim for ≈ 20% fall in haematocrit and adjust fluid rate downwards to avoid
overload - Aim for minimal acceptable urine output (0.5-1ml/kg/hr).
- A urine output > 3 ml /kg /hour indicates Hypervolaemia..
- Fluid replacements are dynamic hence require continuous reassessments.
- No dextrose containing fluid should be used for fluid resuscitation,
- Separate maintenance fluids are usually not required. Glucose/potassium may need to be given separately. Start enteral feeds early.
- All invasive procedures must be performed by most experienced person. If possible, aim for platelets > 50,000/cu mm prior to central line insertion.
- Profuse bleeds may necessitate transfusion of platelets and FFP regardless of lab values: conversely, low platelet counts in the recovering, stable patient may not be an indication for transfusions.
Flow Chart 1-Volume replacement flow chart for a patient with Severe Dengue and a >20% increase in haematocrit. [No Shock](1)
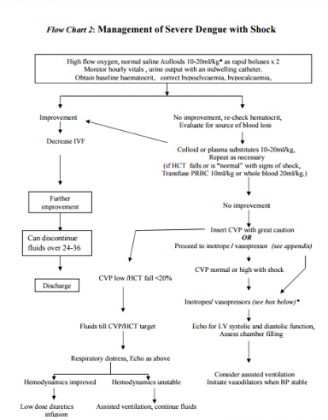
Flow Chart 2: Management of Severe Dengue with Shock
Guidelines by The Ministry of Health and Family Welfare :
Dr. Supraja Chandrashekar and Dr. Rajiv Aggarwal, Department of Pediatrics, Narayana Hrudayalaya, Bangalore.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd