- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
CT head can predict treatment strategy in cerebral edema patients
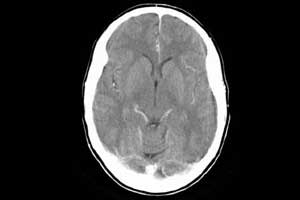
In patients with subdural hematoma with cerebral edema, measurement of head computed tomography (CT) in Hounsfield units (HU) of white matter (WM) might be a useful predictor of outcome and treatment strategy, suggests a new study published in the Scandinavian Journal of Trauma, Resuscitation, and Emergency Medicine. This means that a variable application of CT Head can be extremely useful for evolving a strategy of treatment of subdural hematoma with cerebral edema.
The study was conducted by Hitoshi Yamamura, from Graduate School of Medicine, Hirosaki University, Hirosaki city, Japan, and colleagues to evaluate whether differences in computed tomography measurements in HU of white matter and gray matter can be used as a predictor of outcome in patients with subdural hematoma with cerebral edema. The ability to predict outcome in patients with cerebral edema is important because it can influence treatment strategy.
Severe brain injury results in high morbidity and mortality in trauma patients. If excessive brain edema occurs, it can become uncontrollable and cause secondary brain damage. The assessment of traumatic cerebral edema is difficult. Vasogenic edema caused by the destruction of the blood-brain barrier and increased vascular permeability is a result of serum ingredients leaking outside the capillaries.
Previous studies have reported on the assessment of brain edema using quantitative CT, perfusion CT, magnetic resonance imaging, and transcranial Doppler. However, there are few reports that correlate cerebral edema with the prediction of outcome. The HUof white matter in patients with head trauma correlated with specific gravity values measured in surgical specimens.
For the study, the investigators evaluated 34 patients who had subdural hematoma with cerebral edema following acute closed head trauma and had undergone head CT within a few hours of admission. The patients were divided into the survival (n = 24) group and death (n = 10) group and measured the HU of white matter and gray matter at injury and non-injury sites.
Key Findings:
- There were no significant differences in operation time or blood loss during surgery between the two groups.
- Only the HU of white matter in the injury site of patients in the death group was decreased significantly.
- A cut-off value of 31.5 for HU of white matter showed 80.0 % sensitivity and 99.9 % specificity for death.
HU values in WM may be one factor in the decision-making process that affects patient outcome. Changing the treatment strategy in patients with a low HU value in the WM at the injury site may bring about an improvement in patient outcome.
Based on the findings the researchers concluded that the measurement of HU values in WM at the injury site might be useful as a predictor of outcome in patients with subdural hematoma with cerebral edema. An effective treatment plan needs to be formulated in high-risk patients in whom the HU value of WM is below 31.5.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd