- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Diagnosis And Treatment OF Non-ST elevation Acute Coronary syndrome-Consensus Document
Acute Coronary syndrome (ACS) has evolved as a useful operational term to refer to clinical symptoms that are compatible with acute myocardial ischemia. Non-ST elevation (NSTE) ACS comprises unstable angina (UA) and NSTE myocardial infarction (NSTEMI). The aim of the treatment in ACS is to prevent myocardial necrosis, fatal or non-fatal myocardial infarction (MI), recurrent hospitalization and resultant morbidity and mortality. The CREATE registry(1) data revealed that NSTE-ACS patients take a long time (median 420 minutes) to reach to the hospital in India. Surprisingly, the incidence of NSTE ACS patients was less in this registry in contrast to reports from the west where NSTE ACS is more frequent than STEMI. It is important to note that the mortality of STEMI and NSTE ACS is comparable after 6 months(2). The adverse events in NSTE ACS continue over days and weeks in contrast to STEMI where most events occur before or shortly after the presentation. A large number of detailed guidelines are available from American College of Cardiology (ACC) / American Heart Association (AHA)(3) and European Society of Cardiology(4). An expert consensus document on the management of ischemic heart disease (IHD) in India is also available(5). The current document evaluates and summarizes the currently available evidence on the management of NSTE ACS to assist the Indian physicians in selecting the best management.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for The Diagnosis And Treatment OF Non-ST elevation Acute Coronary syndrome. Following are the major recommendations :
Diagnosis of NSTE ACS :
All patients presenting to a health care provider with symptoms suggestive of ACS should be considered as high priority. For the purpose of this document, an arbitrary division is made to categorize the health care facilities available in India for care of ACS patients (table 1). In big cities centers with varying degree of sophistication are usually available. On the other hand, in parts of India (especially rural) even the basic facilities are not available. Every health care centre should have a functioning ECG machine available 24 hours a day. Health workers at these centers should be trained to interpret the ECG so that treatment can be initiated without delay. Telemedicine (fax, email, and internet) is advancing in our country and a networking between the centers can be of great value.
Definition of terms:
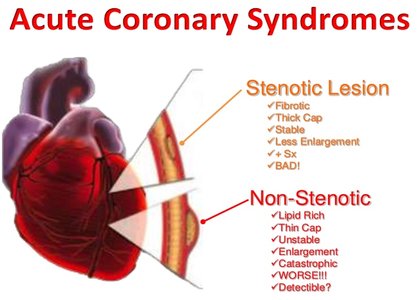
The term, NSTE-ACS includes UA and NSTEMI. These two conditions are closely related whose pathogenesis and clinical manifestations are similar but of differing severity. The clinical presentation depends on the severity of stenosis and the degree of thrombosis. In patients where ischemia is severe, there can be myocardial damage with the release in troponin I (TnI), troponin T (TnT), or CK-MB and the condition is referred to as NSTEMI. If there is no evidence of enzyme elevation, the condition is labeled as UA. It is important to remember that the appearance of biomarkers may be delayed by up to several hours after the onset of ischemic symptoms. The distinction between the terms UA or NSTEMI is retrospective. It is also common to describe patients as Trop T- ve NSTE ACS (UA) or Trop T +ve NSTE ACS (NSTEMI).
Clinical presentation of NSTE ACS:
The clinical presentation of NSTE ACS encompasses a wide variety of symptoms. An accurate history recording is very important. The important points in the history include nature of anginal symptoms, prior history of IHD, sex (male), older age and an increasing number of traditional risk factors. The following clinical presentations are usually included in NSTE ACS(3) .
- Prolonged (> 20 min) anginal pain at rest.
- New onset (de novo) severe angina (class III of the classification of Canadian Cardiovascular Society (CCS)(6) .
- Recent destabilization of previously stable angina with atleast CCS III angina characteristics (crescendo angina) or
- Post MI angina.
The typical clinical presentation of NSTE ACS is retrosternal pressure or heaviness (“angina”) radiating to the left arm, neck or jaw which may be intermittent (usually lasting several minutes) or persistent. These complaints may be accompanied by other symptoms such as diaphoresis, nausea, abdominal pain, dyspnea, and syncope. There are several atypical symptoms and these include epigastric pain, recent onset indigestion, stabbing chest pain, chest pain with pleuritic symptoms, or increasing dyspnea. Atypical complaints are often observed in younger and older patients, in women, and in patients with diabetes.
Clinical assessment of NSTE ACS:
Physical examination: The clinical examination is frequently normal. The presence of tachycardia, heart failure or haemodynamic instability must prompt the physician to expedite the diagnosis and treatment of patients. It is important to identify clinical circumstances that may precipitate or exacerbate NSTE- ACS, such as anaemia, infection, fever and metabolic or thyroid disorders. An important goal of physical examination is to exclude non cardiac causes of chest pain and nonischemic cardiac disorders (e.g. pulmonary embolism, aortic dissection, pericarditis, valvular heart disease) or extra cardiac causes.
Electrocardiogram (ECG): The resting 12 lead ECG is the first diagnostic tool. It should be recorded as soon as possible and immediately interpreted by a qualified physician. The finding of persistent ST elevation suggests STEMI which requires a different treatment. ECG recordings should be repeated at least at 6 and 24 h, and in the case of recurrence of chest pain/symptoms. ECG should be compared with any previously available recordings.
In NSTE ACS, ECG may show ST segment deviation, T wave changes or may remain normal. It should be emphasized that a completely normal ECG does not exclude the possibility of NSTE ACS. In several studies, around 5% patients with normal ECG who were discharged from the emergency department were ultimately found to have acute MI or UA(7). ST segment shifts and T wave changes are the ECG indicators of unstable CAD. The number of leads showing ST depression and the magnitude of ST depression are indicative of the extent and severity of ischemia and correlate with the prognosis(8). ST depression of > 2 mm carries a increased mortality risk. Inverted T waves, especially if marked (greater than or equal to 2mm (0.2 MV) also indicate UA/ NSEMI). Q waves suggesting prior MI indicate a high livelihood of IHD. The utility of ECG becomes less if ECG is abnormal due to pre-existing intraventricular conduction defect or left ventricular hypertrophy (LVH).Ischemia in the left circumflex coronary artery territory is frequently missed in the common 12 lead ECG. It may be detected in lead V4-R, V3- R as well as in leads V7 – V9. These leads should be recorded if clinically indicated.
Biochemical markers : Several biomarkers have been investigated in recent years to be used for diagnosis and risk stratification. Cardiac troponin (CTn) is the biomarker of choice because it is the most sensitive and specific marker of myocardial injury/ necrosis available. Unfortunately, there is a lack of understanding of many of the analytical and clinical issues that govern the use of this important biomarker. The diagnostic cut off for MI using cardiac troponins should be based on the 99th percentile of levels among healthy controls as recommended by the consensus committee(9). All laboratories need to validate their values. The diagnosis of NSTE- ACS should never be made only on the basis of cardiac biomarkers, the elevation should always be interpreted in the context of clinical presentation. Troponin levels usually increase after 3-4 hours. If the first blood sample for CTn is not elevated, a second sample should be obtained after 6-9 h, and sometimes a third sample after 12-24 hours is required. Troponin level may remain elevated upto 2 weeks. Troponin elevation can occur in cardiac and non cardiac conditions including chronic renal failure. In NSTE ACS, elevated CTn values signal a higher acute risk and an adverse long term prognosis. The elevated troponin level is also useful for selecting appropriate treatment. Creatine Kinase MB is less sensitive and specific for the diagnosis of NSTE ACS. However, it remains useful for the diagnosis of early infarct extension (reinfarction) and peri-procedural MI because of its short half-life.
Many other biochemical markers like CRP, NT- Pro BNP, myoglobin are commercially available. At the present time, there use is not recommended for the diagnosis.
Echocardiography: Echocardiography and Doppler examination should be done to assess the global left ventricular function, any regional wall motion abnormality. Echocardiography also helps in excluding other causes of chest pain.
Risk Stratification at presentation:
Many patients with NSTE- ACS require observation/hospitalization in an environment with continuous electrocardiographic monitoring and defibrillation capability. The risk stratification at presentation is useful, however, it is important to understand that patients who are stable initially, may become high risk subsequently or vice versa.
NSTE ACS includes a heterogeneous group of patients with a highly variable prognosis. The risk stratification is necessary for prognosis assessment and treatment. A simple TIMI risk score(10) which takes into consideration clinical variable can be used (Table 2). The TIMI risk score is available at www.timi.org. A low TIMI score <3 usually indicates a low risk and a TIMI score > 3 indicates intermediate or high risk. In general, patients having multiple coronary risk factors, advanced age, rest angina, clinical left ventricular (LV) dysfunction, prior history of percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABGS) indicate a high risk. Elevation of troponin or CK-MB indicates myocyte necrosis and a high risk. It is important to note that the TIMI risk score is just a guide and may not be reliable in young patients. There are other risk models based on PURSUIT trial (11) and GRACE registry(12) .
Data from western countries suggest that patients with acute chest pain might be better served by transport to an adequately equipped facility (category A) than by sending them to a less equipped facility (category B, C or D). It is well documented that early invasive therapy (early coronary angiography followed by appropriate revascularization) is preferable in high risk patients. These patients should preferably be admitted to category A hospitals or promptly transferred to such a facility. If a high risk patient is initially admitted in Category B, C or D hospital, a decision for transportation should be taken. The decision is to be individualized depending on the clinical, social and economic considerations.
Differential diagnosis:
A number of patients evaluated for suspected NSTE ACS are found not to have acute ischemia. This includes patients with non cardiac pain (e.g. pulmonary embolism, musculoskeletal or esophageal discomfort) or cardiac pain not caused by myocardial ischemia (e.g. pericarditis). These patients should be evaluated as dictated by the individual presentation.
Management of NSTE-ACS:
Patients who are awaiting hospitalization are advised to chew non enteric coated aspirin (162 to 325 mg). They may receive sublingual nitrate or GTN spray for pain relief.
Patients with definite or probable NSTE-ACS who are stable should be admitted to an impatient unit for bed rest with continuous rhythm monitoring and careful observation for recurrent ischemia. High risk patients, including those with continuing discomfort and/ or haemodynamic instability, should be hospitalized in a coronary care unit (CCU) and observed for at least 24-48 hours without any major complications.
What not to do ?
- Fibrinolytic (thrombolytic) therapy using streptokinase, urokinase, tenecteplase or any other agent should not be used in patients with UA and NSTEMI. These agents can prove harmful
- Glycoprotein IIb/IIIa agents like abciximab, tirofiban and eptifibatide are mostly useful in patients undergoing percutaneous coronary interventions (PCI). The routine “upstream” use of the agents is not recommended.
Anti- ischemic and analgesic therapy:
All patients must receive medication for relief of pain. Oxygen is useful for initial stabilization particularly in those with hypoxemia.
Topical, oral or intravenous nitrates are recommended for pain relief. Intravenous nitroglycerin (NTG) is particularly helpful in those who are unresponsive to sublingual NTG, in hypertension and in those with heart failure. Nitrates should be used with caution if systolic blood pressure is below 100 mm of Hg.
Morphine sulfate (1 to 5 mg intravenously), if available, is a good option for pain relief in patients whose symptoms are not relieved despite NTG or other anti ischemic therapy. The non steroidal anti inflammatory drugs (NSAIDs) and COX-2 inhibitors should not be administered for pain relief due to increased risk of cardiovascular events(13) .
Oral beta blockers are useful for pain relief. The use of intravenous beta blockers should be avoided particularly in haemodynamically unstable patients. Calcium channel blockers are of utility in vasospastic angina and in patients with contraindications to beta blockade. Other antianginal drugs like ivabradine, trimetazidine, ranolazine and nicorandil have limited role to play.
Antiplatelet agents:
Platelet activation plays a key role in NSTE- ACS and antiplatelet therapy should be administered once the diagnosis is entertained. Aspirin (cyclo oxygenese inhibitor) should be administered to all patients unless contraindicated.
Initial dose of chewed non-enteric aspirin from 162 to 325 mg is recommended. The subsequent dose of aspirin can be 75 to 150mg daily on a long term basis. GI bleeding appears to increase with higher doses.
Clopidogrel is recommended in all patients with an immediate dose of 300 mg followed by 75 mg daily. In patients considered for a PCI, a loading dose of 600 mg is advised to achieve more rapid inhibition of platelet function. Clopidogrel should be maintained for 12 months unless there is an excessive risk of bleeding.
A new antiplatelet agent, belonging to thienopyridine group of ADP receptor inhibitors has recently been investigated in TRITON TIMI- 38 trial(14). Prasugrel reduces the platelet aggregation by irreversibly binding to P2Y12 receptors on the platelets. Prasugrel is a prodrug and has rapid onset of action (1 hour). It is converted to active and inactive metabolites. The active metabolite has half life of about 7 hours. In patients undergoing PCI for ACS, the agent showed lower incidence of ischaemic events when compared to clopidogrel. It was particularly effective in diabetics (4.2% absolute risk reduction for ACS). Bleeding incidence was similar (2.2% vs 2.3%). The agent is correctly recommended for the following patients (1) Patient presenting with STEMI (2) NSTEMI patient with diabetes mellitus or young male patients undergoing PCI (3) Patient with history of stent thrombosis (4) non responders to clopidogrel. This agent is contraindicated in patients with >75 years of age or in patient having history of TIA or any stroke. The loading dose is 60 mg orally. The maintenance dose is 10 mg daily. In patient weighing <60 kg, the maintenance dose has to be reduced to 5 mg daily.
Another new drug, ticagrelor has been found to be superior as compared to clopidogrel in ACS(15) . Ticagrelor is an oral, reversible, non thinopyridine P2Y12 antagonist. This is not a prodrug. This has a more rapid onset of action (30 min) and rapid off sent of action (4-72 hours). In ACS, Ticagrelor was associated with mortality reduction compared to clopidogrel (9.8% vs 11.7%, P=<0.001). However nonfatal bleeding was higher (16.1% vs 14.6%, P=0.0084). The loading dose is 180 mg. Maintenance dose is 90 mg twice daily thereafter.
All patients presenting with ACS/NSTEMI should receive aspiring plus any one of these three (Clopidogrel/Prasugrel/Ticagrelor) agents
The use of GP IIb / IIIa inhibitors has undergone a major change in the current era of high dose clopidogrel and newer anticoagulants. These agents are used either upstream beginning prior to angiography or administered after angiography during the PCI. The upstream use of GP IIb/IIIa inhibitors have considerably reduced. Eptifibatide have not shown efficacy in reducing ischemic events in high risk NSTE-ACS patients when used upstream and maintained during the PCI procedure. In routine practice, these days patients are often taken to catheterization laboratory without prior use of GP IIb / IIIa agent(16). Any of the three agents is used depending on the clinical and angiographic characteristics
Anticoagulants:
Anticoagulation is recommended for all patients in addition to antiplatelet agents(3,4). An increasing number of anticoagulants (previously referred to as antithrombins) are available and include unfractionated heparin (UFH), low molecular weight heparin (LMWH), fondaparinux and bivalirudin.
The choice of anticoagulation depends on the risk of ischemic and bleeding events and choice of the initial management strategy (e.g. urgent invasive, early invasive or conservative).
Enoxaparin (1mg/kg bw twice daily) is a preferred anticoagulant and is a good option in patients treated conservatively or by invasive strategy. Enoxaparin can be stopped within 24 h after an invasive strategy where as it should be administered up to hospital discharge (usually 3 to 5 days) in conservative strategy.
Fondaparinux is recommended on the basis of most favourable efficacy/ safety profile and the recommended dose is 2.5 mg daily(17). This agent causes least bleeding complications. An additional UFH in standard dose of 50-100 U/kg bolus is necessary during PCI due to slightly high incidence of catheter thrombosis.
Bivalirudin is currently recommended as an alternative anticoagulant for urgent and elective PCI in moderate or high risk NSTE ACS(18). Bivalirudin reduces the risk of bleeding as compared with UFH/LMWH plus GP IIb/IIIa inhibitor.
Statins & other drugs:
Statins are recommended for all NSTE ACS patients, irrespective of cholesterol levels. Statin should be initiated early after admission, with the aim of achieving LDLC levels <70 mg/dL. Atorvastatin is usually the preferred agent. High dose (40-80 mg) is used for the initial period (1-2 months). Subsequent dosing is bsed on the target LDL (<70 mg/dL) level.
ACE inhibitors are indicated in patients with reduced LV systolic function in diabetes and all other patient of proven CAD. ARB are indicated in those patients who are intolerant to ACE inhibition.
Coronary Revascularization :
Revascularization for NSTE ACS is performed to relieve angina, ongoing myocardial ischemia and to prevent progression to MI or death. The indications for revascularization and the preferred approach, PCI or CABGS depend on the extent and severity of the lesions, the patient’s condition and co-morbidity(19) .
Coronary angiography :
An invasive strategy always starts with angiography. The indications for urgent and routine early angiography are shown in table 3 and 4.
Those patients who have no recurrence of chest pain, normal serial ECGs, no elevation of troponins and no heart failure are considered as low risk. In these patients, a stress test is advised prior to discharge. Coronary angiography is contemplated, if the stress test is positive.
Conservative and Invasive strategy :
There is a controversy which remains as to the optimal timing between hospital admissions, initiation of medical therapy and invasive evaluation. There are large numbers of randomized controlled trials (RCT) which have addressed this issue. The term invasive strategy refers to coronary angiography and subsequent revascularization within 2 to 24 hours of hospitalization. Conservative strategy (selective invasive) refers to initial medical stabilization followed by angiography and appropriate revascularization, usually within 72 hours or prior to hospital discharge. RCTS have shown that an early invasive strategy reduces ischemic end points mainly by reducing severe recurrent ischemia and the need for re-hospitalization and revascularization(20). This strategy reduces cardiovascular death and MI at up to 5 years of follow-up(21). From the available data, following conclusions can be drawn.
1. High risk/unstable patients benefit most from the early revascularization therapy & these patients should be promptly treated in advanced centers.
2. A systematic approach of immediate angiography is not necessary in patients who are stabilized with a contemporary pharmacological approach. Likewise, immediate transfer of stabilized patients admitted in hospitals without onsite cardiac catheterization facilities is not mandatory, but should be organized within 72 h. Figure 1 provides a flow chart for management of NSTE-ACS patients.
Percutaneous Coronary Intervention (PCI) and Coronary Artery Bypass Grafting (CABG) :
The mode of revascularization is usually based on the severity and distribution of the CAD. The PCI is usually performed for the culprit lesion using drug eluting stents. Significant lesions in multiple vessels can be treated either in same sitting or in staged fashion as considered appropriate. CABG is usually advised for complex CAD not amenable to PCI, left main with triple vessel disease, total occlusions and diffuse disease. It is important to consider the bleeding risk as these patients are on aggressive antiplatelet therapy. The benefits of CABG are greatest after several days of stabilization with medical treatment and stopping the antiplatelet agents.
Long Term Management :
Patients with NSTE ACS after the initial phase carry a high risk of recurrence of ischemic events. Therefore, active secondary prevention is an essential element of long term management. Life style alterations is very important. This is termed as therapeutic life style changes (TLC). Smoking cessation, weight reduction, blood pressure control, management of diabetes, lipid intervention, antiplatelet agents, beta blockers, ACE inhibitors (or ARB) remain extremely important interventions. Isotonic exercise like brisk walk, swimming, cycling, jogging for 30-45 minutes daily or at least 150 minutes weekly should be advised to all these patients. The exercise prescription (type, duration and intensity) should be individualized based on the clinical status of the patient. Lastly psychological factors like anxiety and depression are to be identified and treated(22) .
Table 1 : Type of hospitals / centers treating ACS patients in India.
| Category | Facilities |
| Advanced care with ICCU, catheterization laboratory, PCI and Coronary artery bypass graft (CABG) Surgery. |
| ICCU with trained staff for thrombolysis, CPR, defibrillation, pacing etc. |
| ICU with no specialized cardiac care |
| No ICCU or ICU |
Abbreviations: ICCU = Intensive coronary care unit, ICU = Intensive care unit, CPR = Cardiopulmonary resuscitation. Other as in text.
Table 2 : Indications for urgent coronary angiography and invasive strategy.
- Refractory angina (e.g. evolving MI).
- Recurrent angina despite intense antianginal treatment (associated with ST depression (2 <mm) or deep negative T waves.
- Clinical symptoms of heart failure or haemodynamic instability (‘Shock’).
- Life threatening arrhythmias (ventricular fibrillation or ventricular tachycardia).
Table 3 : Indications for early coronary angiography :
- Elevated troponin levels.
- Dynamic ST or T wave changes.
- Diabetes mellitus, reduced renal function.
- Depressed LVEF < 40%.
- Early post MI angina.
- PCI within 6 months.
- Previous CABG.
- Intermediate to high risk according to risk score.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd