- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Combining Ultrasound & alpha fetoprotein level improve liver cancer detection by 40 Percent
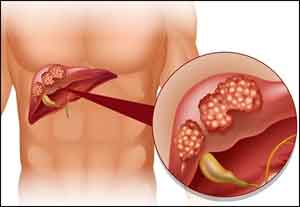
It is well known that Liver Cancer is on the rise and the fastest increasing solid-tumor cancer in the U.S. and earlier detection is important to improving survival of patients.researchers at UT Southwestern’s Simmons Cancer Center found that combining a blood test for high alpha fetoprotein (AFP) level with ultrasound imaging improves detection of early-stage liver cancer by as much as 40 percent.AFP is a plasma protein that is produced in abundance by the liver cells in the fetus. In adults, AFP levels are normally low, but liver cancer can cause AFP levels to rise.The research, a meta-analysis of 32 previous studies, appears in the journal Gastroenterology.
“Liver cancer screening in patients with chronic liver disease has traditionally been performed using an abdominal ultrasound. While ultrasound is readily available and noninvasive, it misses many cancers when they are small,” said Dr. Amit Singal, who holds the David Bruton, Jr. Professorship in Clinical Cancer Research. “Our study found that adding the blood biomarker alpha fetoprotein increased detection of early-stage hepatocellular carcinoma from 45 percent with ultrasound alone to 63 percent using the two tests in combination.
“If the cancer is found early, then we can perform curative therapies, allowing patients to live many years,” said hepatologist Dr. G. Amit Singal, Associate Professor of Internal Medicine and Clinical Sciences with UT Southwestern Harold C. Simmons Comprehensive Cancer Center. “Unfortunately, most liver cancer in the United States is discovered at later stages, when curative treatment is not possible and survival is much worse.”
While the incidence of most cancers is decreasing in the U.S., the incidence of liver cancer has increased by 2.7 percent a year over the last 10 years, according to the NCI, which estimated about 40,700 new cases of liver cancer will be diagnosed in the U.S. in 2018. Risk factors for liver cancer, also known as hepatocellular carcinoma or HCC, include hepatitis C infection, chronic heavy alcohol consumption, and nonalcoholic fatty liver disease related to diabetes and obesity. Symptoms can include upper abdominal pain or swelling, loss of weight or appetite, white chalky stools, and general fatigue.
Liver cancer screening guidelines for patients with cirrhosis vary, with some guidelines calling for just imaging and other guidelines calling for both imaging and AFP measurement.
Collaborators on the study included Dr. Jorge Marrero, Professor of Internal Medicine, and Dr. Adam Yopp, Associate Professor of Surgery, also members of the Simmons Cancer Center, one of just 49 NCI-designated Comprehensive Cancer Centers in the nation and the only NCI-designated Comprehensive Cancer Center in North Texas.
Simmons Cancer Center is among just 30 U.S. cancer research centers to be designated by the NCI as a National Clinical Trials Network Lead Academic Participating Site.
“Our results highlight the importance of continued development and validation of blood-based biomarkers for liver cancer early detection. Most important, our results support a change in clinical practice and the routine use of ultrasound and biomarkers together for liver cancer screening,” said Dr. Singal, Dedman Family Scholar in Clinical Care at UT Southwestern, which is recognizing its 75th anniversary this year.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd