- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo
The American Academy of Otolaryngology-Head and Neck Surgery Foundation has published the Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update) in Otolaryngology-Head and Neck Surgery. The updated guideline provides evidence-based recommendations for healthcare providers on diagnosis and treatment of benign paroxysmal positional vertigo (BPPV) as well as important patient information answering frequently asked questions about BPPV.
BPPV is the most common inner ear problem and cause of vertigo (vertigo is false sense of spinning). It is more common in older individuals with a correspondingly more pronounced health and quality-of-life impact. Older patients with BPPV experience a greater incidence of falls, depression, and impairments of their daily activities. With the increasing age of the U.S. population, the incidence and prevalence of BPPV may correspondingly increase over the next 20 years.
The primary outcome considered in this updated guideline is the resolution of the symptoms associated with BPPV. Secondary outcomes considered include an increased rate of accurate diagnoses of BPPV, a more efficient return to regular activities and work, decreased use of inappropriate medications and unnecessary diagnostic tests, reduction in recurrence of BPPV, and reduction in adverse events associated with undiagnosed or untreated BPPV. Other outcomes considered include minimizing costs in the diagnosis and treatment of BPPV, minimizing potentially unnecessary return physician visits, and maximizing the health-related quality-of-life of individuals afflicted with BPPV.
Major Recommendations :
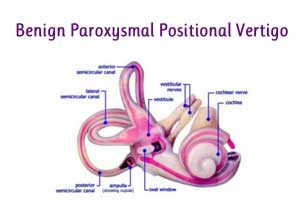
DIAGNOSIS OF POSTERIOR SEMICIRCULAR CANAL BPPV: Clinicians should diagnose posterior semicircular canal BPPV when vertigo associated with torsional, upbeating nystagmus is provoked by the Dix-Hallpike maneuver, performed by bringing the patient from an upright to supine position with the head turned 45° to 1 side and neck extended 20° with the affected ear down. The maneuver should be repeated with the opposite ear down if the initial maneuver is negative
1b. DIAGNOSIS OF LATERAL (HORIZONTAL) SEMICIRCULAR CANAL BPPV: If the patient has a history compatible with BPPV and the Dix-Hallpike test exhibits horizontal or no nystagmus, the clinician should perform, or refer to a clinician who can perform, a supine roll test to assess for lateral semicircular canal BPPV
2a. DIFFERENTIAL DIAGNOSIS: Clinicians should differentiate, or refer to a clinician who can differentiate, BPPV from other causes of imbalance, dizziness, and vertigo.
2b. MODIFYING FACTORS: Clinicians should assess patients with BPPV for factors that modify management, including impaired mobility or balance, central nervous system disorders, a lack of home support, and/or increased risk for falling.
3a. RADIOGRAPHIC TESTING: Clinicians should not obtain radiographic imaging in a patient who meets diagnostic criteria for BPPV in the absence of additional signs and/or symptoms inconsistent with BPPV that warrant imaging.
3b. VESTIBULAR TESTING: Clinicians should not order vestibular testing in a patient who meets diagnostic criteria for BPPV in the absence of additional vestibular signs and/or symptoms inconsistent w
4a. REPOSITIONING PROCEDURES AS INITIAL THERAPY: Clinicians should treat, or refer to a clinician who can treat, patients with posterior canal BPPV with a canalith repositioning procedure (CRP).ith BPPV that warrant testing.
4b. POSTPROCEDURAL RESTRICT-IONS: Clinicians should not recommend postprocedural postural restrictions after CRP for posterior canal BPPV.
4c. OBSERVATION AS INITIAL THERAPY: Clinicians may offer observation with follow-up as initial management for patients with BPPV.
5.VESTIBULAR REHABILITATION: The clinician may offer vestibular rehabilitation in the treatment of BPPV.
6.MEDICAL THERAPY: Clinicians should not routinely treat BPPV with vestibular suppressant medications such as antihistamines and/or benzodiazepines.
7a. OUTCOME ASSESSMENT: Clinicians should reassess patients within 1 month after an initial period of observation or treatment to document resolution or persistence of symptoms.
7b. EVALUATION OF TREATMENT FAILURE: Clinicians should evaluate, or refer to a clinician who can evaluate, patients with persistent symptoms for unresolved BPPV and/or underlying peripheral vestibular or central nervous system disorders
EDUCATION: Clinicians should educate patients regarding the impact of BPPV on their safety, the potential for disease recurrence, and the importance of follow-up.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd