- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Chronic use of Vitamin K anticoagulants and antagonists increases bleeding risk after TAVR
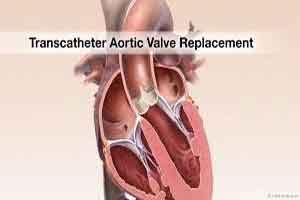
For patients in need of oral anticoagulants after transcatheter aortic valve replacement (TAVR), the chronic use of vitamin K oral anticoagulant (NOACs) as well as vitamin K antagonists (VKAs) is associated with the danger of bleeding, revealed a study published in the Journal of American College of Cardiology, JACC.
The study was conducted to investigate the impact of oral anticoagulation (OAC) type on clinical outcomes 1 year after transcatheter aortic valve replacement (TAVR).
Read more: Five big dangers to be avoided while going for TAVR
The study enrolled 962 consecutive patients who underwent TAVR in 4 tertiary European centers and were discharged on either NOACs or VKAs. By using propensity scores for the inverse probability of treatment weighting (IPTW), the comparison of treatment groups was adjusted to correct for potential confounding. Mean age and Society of Thoracic Surgeons score of the population were 81.3 ± 6.3 years and 52.5% were women. A balloon-expandable valve was used in 62.7% of cases.
The primary outcome of interest, the combined incidence of all-cause mortality, myocardial infarction, and any cerebrovascular event at 1-year after TAVR, was 21.2% with NOACs versus 15.0% with VKAs. The 1-year incidence of any Bleeding Academic Research Consortium bleeds and all-cause mortality was comparable between the NOAC and VKA groups, 33.9% versus 34.1% and 16.5% versus 12.2%, respectively. The outcome showed that NOACs had a greater risk of all-cause mortality composite, MI, or any cerebrovascular event with a considerable borderline difference.
The authors concluded that chronic use of both NOACs and VKAs among patients in need of oral anticoagulant after TAVR are similar regarding 1-year bleeding risk. However, the higher ischemic event rate was observed with NOACs which requires further investigation.
TAVR, although has become one of the most common cardiac surgeries in recent years and is on the verge of becoming the standard of care for patients with severe aortic stenosis at enhanced danger of surgery. But, concerns exist about the bleeding risks.
For further reference, click on the link
DOI: 10.1016/j.jcin.2019.03.003

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd