- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Case of Myasthenic crisis following iodinated contrast material aspiration: a report

Dr B. V. K. M. Bopeththa and colleagues at Emergency Medicine, Teaching Hospital Peradeniya, Peradeniya, Sri Lanka have reported a case of Myasthenic crisis following iodinated contrast material (iohexol) aspiration that has appeared in the Journal of Medical Case reports.
The number of contrast media-related procedures is ever increasing due to the widespread availability of theoretically safe, low osmolar iodinated contrast material. Although intravenously administered contrast is known to precipitate a myasthenic crisis, oral contrast aspiration as a causative factor is not yet documented as such.
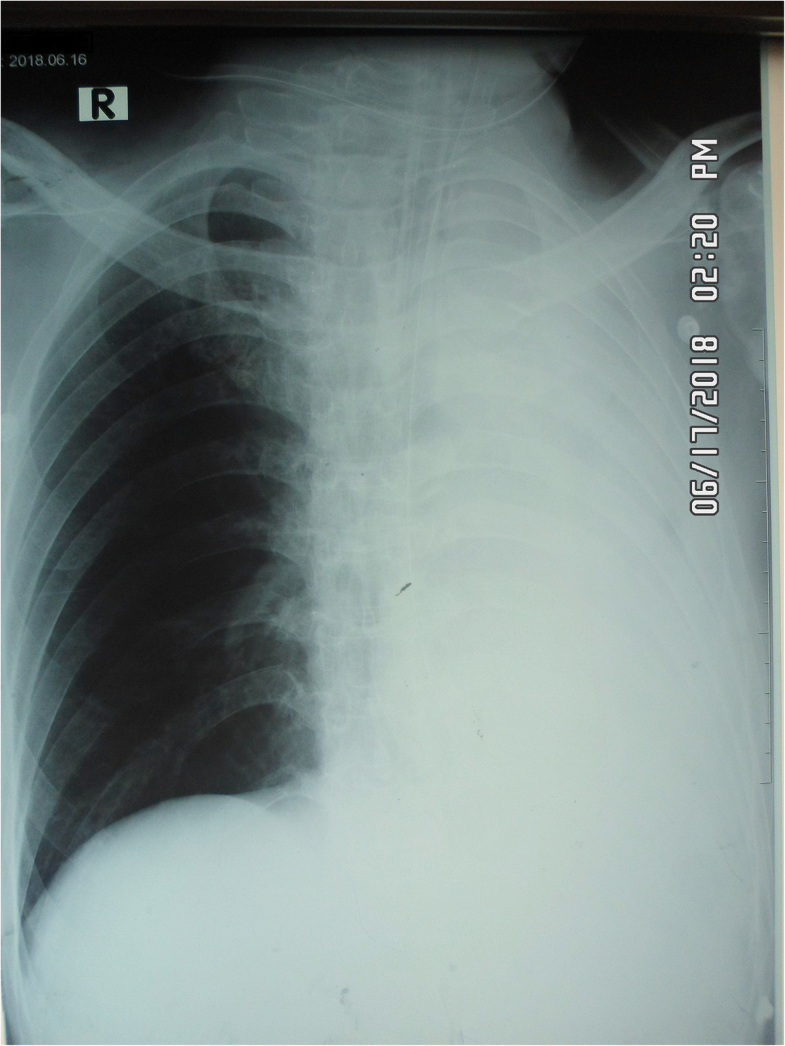
A 48-year-old Sinhalese man with myasthenia gravis was presented to the department of radiology of a tertiary care hospital for upper gastrointestinal (GI) contrast study, for further evaluation of progressive dysphagia. Myasthenia gravis was diagnosed in May 2016 and he underwent thymectomy in November 2016 for thymic hyperplasia. From the point of diagnosis, he had two episodes of myasthenic crisis, precipitated by lower respiratory tract infections that required mechanical ventilatory support. Thereafter, he was on regular pyridostigmine, 50 mg/6 hourly, mycophenolate mofetil (MMF) 500 mg twice daily, and orally administered prednisolone therapy. He was able to perform his daily routines of life with negligible support. Meanwhile, he developed progressive dysphagia for solids initially and then for liquids for a 3-month duration. He was evaluated by a neurologist and referred to the surgical team for upper GI endoscopy. Since that was also uneventful, he was referred to our radiology unit for a contrast study. On admission to the radiology unit, he had normal respiratory parameters and his limb muscle power was grade 5/5. Due to the possible risk of aspiration, 10 ml of iohexol (Omnipaque™) was given under fluoroscopy guidance. As the contrast material had directly entered his right main bronchus, the procedure was abandoned and he was transferred to the accident and emergency treatment unit (ETU). Although he was able to maintain his air oxygen saturation above 90% with high flow oxygen via non-rebreather mask, an effort of breathing drastically dropped 45 minutes after admission to the ETU including dropping of respiratory rate to 10 breaths per minute. Despite continuous treatment with nebulized salbutamol and intravenously administered metronidazole 500 mg stat dose, he eventually required endotracheal intubation with 3 mg midazolam and 10 mg atracurium administered intravenously. There was a drooping of eyelids, but it was very difficult to assess limb muscle power before intubation. According to the clinical scenario, the diagnosis of respiratory distress due to contrast aspiration was made and he was transferred to the ICU. Following admission, the diagnosis was questioned as there were no significant chest X-ray (CXR) abnormalities to cause the high degree of respiratory distress, except right apical segment collapse. He was then evaluated by a neurologist and the diagnosis was revised to myasthenic crisis, possibly due to aspiration pneumonitis caused by aspiration of contrast. Hence, intravenously administered immunoglobulin 20 g daily for 5 days was commenced with an increased dose of pyridostigmine 60 mg 6 hourly, MMF 750 mg twice daily, and prednisolone 40 mg daily. Although there was no clinical, microbiological, or serological evidence of infection, considering the high possibility of potential development of sepsis, intravenously administered ceftriaxone 1 g 8 hourly was initiated. In addition, there were no electrolyte abnormalities acting as a precipitant of myasthenic crisis. Mechanical ventilation was continued in a synchronized intermittent mandatory mode with fraction of inspired oxygen (FiO2) of 50%, positive end-expiratory pressure (PEEP) of 5 cmH2O, and pressure support 10 cmH2O. Respiratory support was gradually reduced over a 72-hour period as there was a remarkable improvement in his respiratory mechanics with the treatment. Meanwhile, there was a sudden de-saturation with evidence of subcutaneous emphysema on the right side of his neck and a subsequent CXR revealed the complete collapse of his left lung, a hyperinflated right lung with slightly increased translucency on the same side, with right-sided subcutaneous air (Fig. 1). CXR findings raised the suspicion of right-sided pneumothorax. Since the cause of subcutaneous emphysema was occult in the CXR, non-contrast computed tomography (NCCT) of his chest was done and revealed total left lung collapse with ipsilateral mediastinal shift and left loculated pneumothorax.
 Courtesy Journal of Medical Case Reports
Courtesy Journal of Medical Case ReportsSubsequent bronchoscopy was negative. However, with regular chest physiotherapy, lung collapse improved. He was then gradually weaned off the ventilator and transferred to the general medical ward for a continuation of care. Following an 18-day hospital stay, he was successfully discharged from the hospital with a tailing off dose of prednisolone. However, due to the high possibility of aspiration, he was advised to keep the nasogastric tube. Two weeks following discharge, during the first clinic visit, he was ambulant showing an improvement in swallowing. The nasogastric tube was removed and regular follow-up was planned.
For further reference log on to :
https://doi.org/10.1186/s13256-019-2114-8

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd