- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Case of Microfilaria with unusual presentation of Swelling on the Arm

Dr Supriya M Paranjpe at Department of Microbiology, Seth G.S. Medical College & KEM Hospital, Parel, Mumbai, India and colleagues have reported a case of Microfilaria with an unusual presentation of Swelling on the Arm. The case has appeared in the Journal of Medical Case Reports.
A 35 years old male presented with a swelling of approximately 3×2.5 cm on the antero-medial aspect of the right arm since four months [Fig.1]. The swelling was not associated with fever, pain or redness. There was no history of trauma, surgery or travel. A differential diagnosis of lipoma was made. As the patient did not have any signs and symptoms of filarial infection, filariasis was not clinically suspected.

A complete blood count revealed a total count of 6.79×103/µL, neutrophils (58%), lymphocytes (30.4%), monocytes (3.3%), eosinophils (8%), basophils (0.3%), red blood cell count 4.11×106/µL with hemoglobin 14.8 g/dL. The other investigations such as liver function test, renal function test and blood sugar were normal. HIV test was non-reactive. Ultrasound (USG) of the swelling reported an approximately 5 cm tubular hypo-echoic lesion in the antero-medial aspect of the right arm communicating with the basilic vein. Deep venous system of the arm appeared normal. The lesion was localized only to the subcutaneous plane. Underlying muscle appeared normal. The USG findings were suggestive of the basilic vein thrombophlebitis with a group of lymph nodes compressing the basilic vein.
Fine needle aspiration cytology (FNAC) of the swelling was advised. FNAC of the swelling was done under aseptic conditions, by 23 gauge needle attached to 10 ml disposable syringe. Slides were air dried, fixed, with ether alcohol and stained by haematoxylin and eosin. Fine needle aspiration cytology (FNAC) of the swelling revealed few lymphocytes, occasional eosinophils and cyst macrophages against a background of fluid. Many sheathed microfilariae with central column of nuclei were also noted.
The patient was referred for a DEC (diethylcarbamazine (DEC) provocation test. The patient was advised to take single dose of diethylcarbamazine 100 mg orally to induce appearance of microfilariae (which has nocturnal periodicity), in the peripheral blood in the daytime. Blood sample was collected 30 minutes after diethylcarbamazine (DEC) administration and was examined by three methods. (i) Examination of unstained preparation: Two drops of blood were taken on a clean grease free slide and cover slip was put over it. The slide was examined under low power and then high power objective. Microfilariae were seen as a transparent and sheathed worm with rounded anterior end and pointed tail end [Fig.2]. (ii) Examination of stained preparation: Thin and thick film of blood was prepared. Thick film was dehemoglobinised by immersing the slide in water and intermittent rocking for few seconds. The slide was dried, fixed in methyl alcohol and stained with Leishman stain. Microfilariae were seen in both the thin and thick films. Features like excretory and anal pores and absent body nuclei in tail tip were also observed [Fig.3]. (iii) Knott’s concentration method: 1 ml volume of anti-coagulated blood was mixed with 10 ml of 2% formalin, centrifuging the preparation. The supernatant fluid was decanted and the sediment was drawn into a film which was air dried, fixed and stained with Leishman stain. On examination, microfilaria was detected with features seen as those in the previous method.
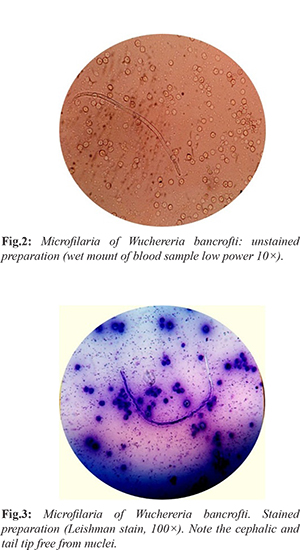
W. bancrofti was confirmed by absence of nuclei in cephalic and tail end and was thus differentiated from Loa loa. Thus correlating the cytological and microscopic findings it was diagnosed as a case of subcutaneous nodule on the antero-medial aspect of the arm due to filariasis caused by W. bancrofti. On follow up, the patient showed improvement with no microfilariae in peripheral blood on repeat DEC provocative test after 2 months.
basilic vein thrombophlebitisfilarial infectionFine needle aspiration cytologyHIV testJournal of Medical Case Reportslymph nodesmethyl alcoholmicrofilariared blood cellswellingtraumaW bancrofti
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd