- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Case of DIC presenting as symmetrical peripheral gangrene: a report

Dr Vineet Jain at Department of Medicine, Hamdard Institute of Medical Sciences & Research (HIMSR), New Delhi, India and colleagues have reported a rare case of Disseminated intravascular coagulation presenting as symmetrical peripheral gangrene .The case has appeared in the Journal of Medical Case Reports.
A 44-year-old Indian man, resident of New Delhi, India, a known alcoholic, presented with a 2-day history of fever. His fever was 39.44 °C (103 °F), continuous and was associated with chills and rigors. Two days after onset of fever, he developed painful bluish discoloration of both hands and feet. There was no history of bluish discoloration of tongue, breathlessness, or chest pain. There was no history of hypertension, diabetes, malaria, or any chronic illness in this patient.
On clinical examination he was conscious, oriented, and well hydrated. His pulse was 80 beats per minute. Bilateral radial and dorsalis pedis arteries were feeble with bluish discoloration of fingers (Fig. 1) and toes. His other peripheral pulses (carotid and femoral arteries) were palpable but low in volume. Blood pressure was not recordable in both upper limbs and was 90/60 mmHg in both his lower limbs. Both hands and feet were pale and cold to touch and there was marked tenderness in both forearm and calf muscles. There was no cyanosis of tongue or nose and there was no lymphadenopathy. The rest of the clinical examination was unremarkable.
A provisional diagnosis of symmetrical arterial ischemia/obstruction with impending gangrene was made and he was investigated further.
His hemoglobin was 15.9 g/dL (13–18 g/dL), hematocrit 44.8% (40–50%), total leukocyte count 3.9 × 103/mm3 (4–11 × 103/mm3), and platelet count 8000/mm3(150,000–400, 000/mm3). Renal and liver functions were deranged with blood urea 90 mg/dL (15–45 mg/dL), serum creatinine 2.6 mg/dL (0.5–1.5 mg/dL), serum bilirubin 12.70 mg/dL (0.2–1.2 mg/dL), direct bilirubin 9.86 mg/dL (0.0–0.2 mg/dL), indirect bilirubin 2.84 mg/dL (0.0–1.0 mg/dL), albumin 2.4 g/dL (3.4–5.0 g/dL), aspartate transaminase 116 IU/L (5–40 IU/L), alanine transaminase 46 IU/L (5–40 IU/L), and alkaline phosphatase 116 IU/L (45–116 IU/L). His prothrombin time was 27.3 (control value 13); his international normalized ratio (INR) was 2.30. His random blood sugar was 64 mg/dL and arterial blood gas analysis was unremarkable.
Arterial Doppler of both upper and lower limbs was normal and did not reveal any thrombus in any of the arteries. Radiography of his chest was normal.
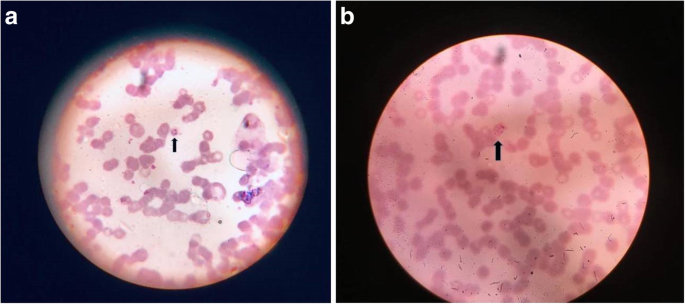
A peripheral smear (using Giemsa stain) for malaria revealed ring forms and schizonts of P. vivax (Fig. 2a, b). The level of parasitemia in thick blood films was 2+ which corresponds to 11–100 parasites/100 thick films fields examined. This was later confirmed by a malaria antigen rapid diagnostic test (RDT) which detected P. vivax lactate dehydrogenase (LDH) ruling out a mixed infection with P. falciparum. NS1 antigen and dengue serology were negative. Fibrin degradation products was > 20 μg/ml (< 5). His D-dimer level was 26.52 μg/mL (< 0.5) fibrinogen-equivalent units. Tests for antinuclear antibodies and antineutrophil cytoplasmic antibodies were negative.
He was treated with injection artesunate 120 mg followed by lumefantrine 480 mg and artemether 80 mg two times per day for 3 days followed by primaquine 15 mg (0.25 mg/kg) per day for 14 days; his glucose-6-phosphate dehydrogenase (G6PD) levels were normal. He also received six units of platelet concentrates, along with cautious use of intravenously administered fluids.
The response to this line of treatment was striking and gratifying. He became afebrile by the second day of admission and by the third day all peripheral pulses were well felt along with normalization of blood pressure in all his limbs. Bluish discoloration of both hands and feet started fading by the third day and pain disappeared in the involved regions. His laboratory investigations normalized by sixth day of admission following treatment except for slightly raised bilirubin. He was discharged and no clinical or laboratory abnormality was reported on follow-ups at 2 weeks and 6 weeks.
For more details click on the link: https://doi.org/10.1186/s13256-019-2117-5

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd