- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Case of Corneal ectasia following cataract extraction surgery in patient with keratoconus: a report
Dr Georgios Labiris at the Department of Ophthalmology, University Hospital of Alexandroupolis, Dragana, Alexandroupolis, Greece and colleagues have reported a rare case of Corneal ectasia following cataract extraction surgery in a patient with keratoconus.The case has appeared in the Journal of Medical Case Reports.
The patients with keratoconus have a genetic predisposition to corneal ectasia which may not be activated or reactivated unless an additional stressful event triggers the disease. Triggering factors are sources of reactive oxidative stress; among them, mechanical trauma (vigorous eye rubbing, poorly fit contact lenses), exposure to ultraviolet light, and atopy/allergies.
A 38-year-old Caucasian man was referred to out patient service from his physician due to bilateral cataract. His systemic medical and family history was negative. He was receiving no medication; he did not smoke tobacco or consume alcohol; he worked as a clerk in a bank. His ophthalmological history indicated bilateral KC with myopic astigmatism, for which he received CXL (Dresden protocol) in both his eyes 5 years prior to his visit to our hospital. According to his medical note, ever since the CXL, KC had been stable.
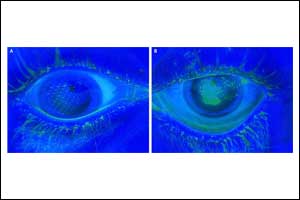
He underwent a thorough systemic examination that did not reveal any pathological signs. On admission, his heart rate was 70 beats per minute, his blood pressure was 120/70 mmHg, and he had a normal body temperature. Subsequently, he underwent a full ophthalmological examination including slit-lamp biomicroscopy, optical biometry, Scheimpflug tomography, corneal biomechanical assessment, and fundus examination. During the examination, we confirmed advanced centrally located cataract and: (a) index of height decentration (IHD) = 0.019; (b) index of vertical asymmetry (IVA) = 0.33, which are common signs of post-CXL corneas (Fig. 2). His best spectacle-corrected visual acuity (BSCVA) was count fingers (CF) for both eyes. Preoperative flat keratometry (K1) reading was 40.5 diopters (D), steep keratometry (K2) reading was 41.8 D, astigmatism was 1.3 D, and thinnest corneal thickness (TCT) was 503 μm. His corneal hysteresis (CH) was 8.2 while his corneal resistance factor (CRF) was 7.5, which were consistent with KC and post-CXL corneas. His fellow eye demonstrated K1 = 40.9 D, K2 = 41.9 D, IHD = 0.041, IVA = 0.67, CH = 8.0, and CRF = 7.3. Fundus examination turned negative for both eyes.
The authors decided to propose phacoemulsification surgery for his right eye with an intraocular lens (IOL) implantation. Our patient consented to the operation and we proceeded to uncomplicated phacoemulsification with Alcon Infiniti® Vision System platform (80% continuous amplitude with 350 mmHg vacuum limit and 40 mL/minute aspiration flow rate) with 2.2 clear-corneal main incision and two contralateral stabs. A foldable hydrophilic acrylic IOL (SN60WF, Alcon Laboratories, Inc.) was implanted, and our patient was released the same day with a fixed combination of tobramycin 0.3% and dexamethasone 0.1% (FCTD) (Tobradex; Alcon, Greece) six times daily, gradually tapered over a month. His uncorrected visual acuity (UVA) during the first week was improved to 20/32, BSCVA = 20/25, his intraocular pressure (IOP) was 17 mmHg, and slit-lamp biomicroscopy revealed minor endothelial striae that were attributed to the phacoemulsification energy.
Three months following the phacoemulsification, he was referred again to our hospital from his physician due to constantly increasing myopic astigmatism. We performed a Scheimpflug tomography and we detected significant corneal thinning, corneal protrusion (K1 = 47.6 D, K2 = 50.2 D), TCT = 319 μm (Fig. 4), and manifest refraction (− 5.00 sph − 2.50 cyl 180o). His UVA in his right eye was CF, while his BSCVA dropped to 20/32. All tomographical signs suggested potential corneal ectasia. To our surprise, ocular response analyzer evaluation confirmed a biomechanical destabilization of the cornea with a significant reduction of the CH = 6.6 and CRF = 7.2, (Fig. 3, waveform #1). Six months following the cataract extraction surgery, both Scheimpflug tomography and ocular response analyzer demonstrated slightly improved tomographical and biomechanical indexes; however, they were fully indicative of postoperative ectasia (K1 = 45.5 D, K2 = 48.3 D), astigmatism = 2.8 D, CH = 6.8, CRF = 7.5, TCT = 318 μm (Figs. 3 and 5, waveform #2). His UVA in his right eye remained CF, while his BSCVA was 20/32. Non-significant changes in the K1 and K2 readings could be detected in his left eye (K1 = 40.8 D, K2 = 42.0 D) and in BSCVA which did not change and remained CF.
Journal Information: Journal of Medical Case Reports
For more details click on the link: https://doi.org/10.1186/s13256-019-2238-x

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd