- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Carcinoma Oral Cavity - Standard Treatment Guidelines
Tumours of lips and oral cavity often present a significant problem to the surgeon with regards to early diagnosis and staging, access for resection and reconstruction of both soft tissues and bone. Tumour of lips are now included within the UICC classification for oral cavity tumours.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Benign Lesions of Larynx. Following are the major recommendations :
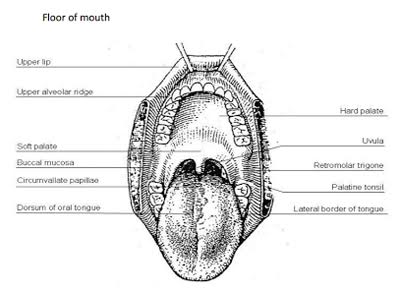
Surgical Anatomy
Anatomic
Sites and Subsites for Lip and Oral Cavity
Lip
External upper lip (vermilion border)
External lower lip (vermilion border)
Commissure
Oral Cavity
Buccal mucosa
Mucosa of upper and lower lips
Cheek mucosa
Retromolar areas
Bucco-alveolar sulci, upper and lower (vestibule of mouth)
Upper alveolus and gingiva (upper gum)
Lower alveolus and gingiva (lower gum)
Hard palate
Tongue
Dorsal surface and lateral borders anterior to circumvallate papillae (anterior two thirds)
Inferior (ventral) surface
Epidemiology
The lip is the most common site of cancer in the mouth. It is most common in white people and approximately 93% of the tumour present in the lower lip and the male to female ratio 80:1. The most common tumour is squamous cell carcinoma.
In case of oral cavity cancer an estimated 387500 new cases are diagnosed annually worldwide. It constitutes 30-40% of head and neck cancer in India and the country ranks among the top few in the world in the incidence of these cancers. Buccal mucosa is a common subsite in Indian population, probably aided by the chewing habit that is prevalent in this country. In India, buccal mucosa cancer is the most common cancer in men and third most common cancer in women. The oral cancers assume importance in the cancer control programme of the country because of its impact on the overall health of the population as well as potential as a target for early detection and prevention
Predisposing Factors
- Smoking tobacco is a potential risk factor for oral cancer. An interaction occurs between redox-active metals in saliva and the low reactive free radicals in cigarette smoke. The incidence of oral cavity cancers in persons who smoke is approximately 6 times that of those who do not. It causes sequential histological changes in oral mucosa. Over a prolonged period of exposure, these changes eventually lead to neoplastic transformation.
- Alcohol consumption- alcohol beverages may contain carcinogens or pro-carcinogens including nitrosamine and urethane contaminants and ethanol. Ethanol is metabolized by alcohol dehydrogenage and to some extent by cytochrome p450 to acetaldehyde, which may be carcinogenic. The combined effect of alcohol and cigarette is synergistic. The risk for a person who smokes and drink is 15 that of an individual who neither habit.
- Betel nut chewing- it cause damage to buccal mucosa.
- Dental caries
- Hot spicy food
- Chronic glossitis
- Malnutrition
- Poor oral hygiene
Precancerous Conditions
Oral cancer can occur as denovo or on existing pre-malignant conditions. These include-
1. Leucoplakia- this is a clinical term without a definitive histological definition. Leukoplakia is a white mucosal based keratotic plaque that cannot be wiped free from the underlying tissue. It is defined as white patch in oral mucosa that cannot be characterized clinically or pathologically as any other disease. Most frequent sites are the buccal mucosa and the commissures. Leukoplakia with epithelial dysplasia (20%) is found to have greater chance of malignant transformation. Only 6% of lesion eventually progressed to SSC. A biopsy is indicated if the lesion is suspicious.
2. Erythroleukaplakia- the associated risk for malignant transformation is greater than leukoplakia.
3. Submucosal fibrosis- most frequently encountered in individuals who chew betel nut, or poor oral hygiene, or periodontitis. The risk of developing oral carcinoma is 7.6% over a 10 year period.
4. Lichen planus- it also been associated with the development of oral carcinoma.
Symptoms of Oral Cancer-
- White or red patches in your mouth
- A mouth sore that won't heal
- Bleeding in mouth
- Loose teeth
- Problems or pain with swallowing
- A lump in neck
- An earache
Differential Diagnosis
1. Chronic non-healing ulcer in oral cavity- characteristic findings in favor of malignant ulcer are-
- Seen in elderly
- Usually seen at margin and ant 2/3 of tongue
- Single or multiple
- Raised, rolled out and everted edge
- Floor covered with necrotic debries and looks dirty gray
- Discharge is offensive
- Painless initially but painful later wit Otalgia due to involvement of lingual nerve
- Associated with lymph node enlargement and it is hard in consistency
2. Pre-malignant conditions like leukoplakia and erytholeukoplakia
TNM Staging
T1: Tumor 2 cm or less in greatest dimension
T2: Tumor more than 2 cm but not more than 4 cm in greatest dimension
T3: Tumor more than 4 cm in greatest dimension
T4a: Moderately advanced local disease.
Lip: Tumor invades through cortical bone, inferior alveolar nerve, floor of mouth, or skin of face, ie, chin or nose
Oral cavity: Tumor invades adjacent structures only (eg, through cortical bone [mandible, maxilla], into deep [extrinsic] muscle of tongue [genioglossus, hyoglossus, palatoglossus, and styloglossus], maxillary sinus, skin of face)
T4b: Very advanced local disease. Tumor invades masticator space, pterygoid plates, or skull base, and/or encases internal carotid artery
Prognostic Markers
Various features of the cancer allow to prognosticate the outcome of the treatment.
- Pathological involvement of cervical node
- T-stage
- Tumour thickness- chance of nodal metastasis is maximum with tumour thickness >5mm.
- Surgical margins- the chance of treatment failure is high when the margin of resection is closed (<5mm) or involve.
Evaluation
1. History & Examination - Almost 90% of the cancers are of squamous cell variety. Buccal mucosa is the most common site affected in India. The sump area or 'coffin corner' at the posterior tongue/ floor of the mouth is a common site for cancer but may be missed by cursory inspection. So, a through history and physical examination is very important for its early detection.
2. Biopsy can be taken at OPD if lesion is large otherwise it can be taken under GA.
3. Endoscopies can be carried out to rule out other synchronous malignancy.
4. Chest imaging, CT/MRI if indicated.
5. Preanesthesia studies.
6. Dental evaluation.
Treatment protocol
1. For T1–2, N0 disease
a) Excision of primary (preferred) ± unilateral or bilateral selective neck dissection.
- If it is associated with No adverse features like (extracapsular nodal spread, positive margins, pT3 or pT4 primary, N2 or N3 nodal disease, nodal disease in levels IV or V, perineural invasion, vascular embolism) then only follow up is required.
- If it is associated with one positive node without adverse feature RT can be given optional. If it is associated Adverse features then planned for Re-excision or Chemo/RT and follow up.
b) An alternative to surgery - External-beam RT ± brachytherapy 70 Gy to primary 50 Gy to neck at risk.
- If pt came with No residual disease then follow up is required.
- If pt landed with Residual disease then Salvage surgery can be better choice.
2. For T3, N0 disease Excision of primary and reconstruction as indicated and unilateral or bilateral selective neck dissection is the treatment of choice.
- If it is associated with No adverse features like (extracapsular nodal spread, positive margins, pT3 or pT4 primary, N2 or N3 nodal disease, nodal disease in levels IV or V, perineural invasion, vascular embolism) RT can be given optional.
- If it is associated adverse features then planned for Re-excision or Chemo/RT and follow up.
3. T4a, Any N; T1-3, N1-3 disease Surgery is treatment of choice.
a) For N0, N1, N2a-b, N3 Excision of primary, ipsilateral comprehensive neck dissection ± contralateral selective neck dissection (reconstruction as indicated) can be considered.
b) For N2c (bilateral) disease Excision of primary and bilateral comprehensive neck dissection (reconstruction as indicated) can be planned.
- In both cases if there are No adverse features RTc (optional) can be given and then follow up.
- If it is associated Adverse features (extracapsular nodal spread, positive margins, pT3 or pT4 primary, N2 or N3 nodal disease, nodal disease in levels IV or V, perineural invasion, vascular embolism) then planned for Re-excision or Chemo/RT and follow up.
Treatment Protocol for Pre-Malignant Lesion
1. Full history and examination.
2. Biopsy
a) Biopsy negative- Discharge
b) Leukoplakia and other pre-malignant lesion- Excision biopsy, Laser etc- Follow up in H & N clinic
c) Other pathology like Lichen planus, candidiasis- Oral medication
d) Biopsy positive- EUA and imaging- Definitive treatment
Preventive Measures
- Don't smoke. Don't drink more than 1 or 2 alcoholic drinks, if any, a day
- Sick immediate attention to doctor in chronic non-healing ulcer mouth
- Maintain adequate oral/dental hygiene.
Guidelines by The Ministry of Health and Family Welfare :
Dr J M Hans Ex-HOD Dept. of Otorhinolaryngology Dr.RML Hospital New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd