- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Cancer cervix-Standard Treatment Guidelines
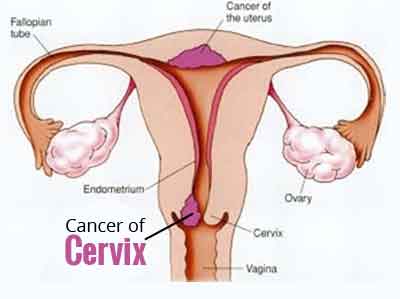
Cervical cancer is major world health problem for the women. It is the third most common cancer worldwide (1,2) and is the most common cancer among women in India. Every year about 1,32,000 Indian women are diagnosed of cervical cancer and over 80,000 die of the disease (IARC estimates) (3). In recent years, molecular biology has firmly established a causal relationship between persistent infection with high risk human papilloma virus (HPV) genotypes and cervical cancer. Other epidemiological risk factors are early age of onset of coitus, larger number of sexual partners , smoking, high parity,prolonged contraceptive use, sexually transmitted disease and chronic immunosuppression(4) Cervical cancer progresses slowly from preinvasive cervical intraepithelial neoplasia to invasive cancer. It is a preventable cancer and successfully treatable when diagnosed in early stages where reported survival is more than 90%(5).
It is important to render the optimal treatment to these women to achieve the best survival as well as the quality of life. Gynae Oncologist / Gynaecologist trained in Oncology for at least one year in prestigious cancer center should preferably treat these patients jointly with Radiation Oncologist & Medical Oncologist as the management includes complex surgeries and multimodality team approach.
Considerations have been given to the available facility for investigations and the expertise available for treating cervical cancer in developing these guidelines.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Cancer cervix.
Following are the major recommendations :
When to suspect: Symptoms
Precancerous condition & early stage cervical cancer have no symptoms. Following symptoms require proper evaluation for cervical cancer
Increased vaginal discharge
Contact Spotting / Bleeding
Inter menstrual Bleeding
Postmenopausal Vaginal Bleeding
Pain Lower Abdomen &
Backache
Incidence of the cervical cancer in our country
1, 32,000 Cases of cervical cancer are diagnosed every year.
Mortality : 80,000 cases die of cervical cancer every year.( IARC )(3)
Differential diagnosis
Cervical Polyp, Endocervical / Endometrial polyp presenting at cervix., cervical Leiomyoma & Condyloma cervix
Prevention & Counseling
Primary prevention
HPV Vaccination :
Vaccination against HPV-16 and HPV-18 reduces incident and persistent infections with efficacy of 91.6% (95% CI, 64.5–98.0) and 100% (95% CI, 45–100), respectively.(6)
Barrier protection and/or spermicidal gel during sexual intercourse and avoiding the following high risk epidemiological factors.(4)
Cigarette Smoking
High Parity
Long-term use of oral contraceptives (>5 Years)
Secondary Prevention
Screening via Gynecologic Examinations and Cytologic Screening
Precancerous condition have no symptoms and is discovered on routine screening tests & usually diagnosed on colposcopic directed biopsy examination.(7)
Regular gynecologic examinations
Cytologic test (Papanicolaou smear)
HPV DNA Testing
In low resource settings the following alternative approaches of VIA & VILI can be implemented effectively where Pap Test is not feasible for the mass screening because of the lack of trained manpower, infrastructure, quality assurance & the cost involved (8)
Visual Inspection of cervix with Acetic Acid (VIA)
VILI ( Visual Inspection of cervix with Lugol’s Iodine)
Secondary prevention : Treatment of the premalignant cervical lesions.
Estimates from population studies in the developed countries suggest that screening using the Pap Test may decrease cancer incidence and mortality by more than 80%.(9)
Optimal Diagnostic Criteria, Investigations, Treatment & Referral criteria
Situation 1 : At Secondary Hospital / Non- Metro situation : Optimal Standards of treatment in situations where technology and resources are limited.
Diagnostic criteria
History
Physical Examination & gynaecological examination including Per Vaginal & Per Rectal Examination.
Definitive Diagnosis : On histopathology of cervical growth/ lesion biopsy either punch / knife / Colposcopic Biopsy / Endocervical curettage / Diagnostic LEEP Cone biopsy ( indicated for diagnosis of microinvasive cervical cancer ).
Investigations
Histopathology/ Pathologic review
Blood : Hb%, CBC, KFT, LFT, Blood Sugar F & PP, HbsAg, HIV
Imaging
X-ray Chest,
USG Whole abdomen & TVS ( For Measuring the tumor size) or
CECT/ MRI Whole abdomen when facility exists / IVP (Clinically Parametrial involvement is suspected and the CT facility is not available )
EUA,Cystoscopy / Sigmoidoscopy when parametrial / bladder / rectal involvement is suspected.
Other Investigations if required based on comorbid conditions.
Cancer Cervix is staged as per the FIGO Staging 2009(9)
Carcinoma of the cervix uteri
| Stage I | The carcinoma is strictly confined to the cervix (extension to the corpus would be disregarded) |
| IA | Invasive carcinoma which can be diagnosed only by microscopy, with deepest invasion ≤5 mm and largest extension ≥7 mm |
| IA1 | Measured stromal invasion of ≤3.0 mm in depth and extension of ≤7.0 mm |
| IA2 | Measured stromal invasion of >3.0 mm and not >5.0 mm with an extension of not >7.0 mm |
| IB | Clinically visible lesions limited to the cervix uteri or pre-clinical cancers greater than stage IA |
| IB1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
| IB2 | Clinically visible lesion >4.0 cm in greatest dimension |
| Stage II | Cervical carcinoma invades beyond the uterus, but not to the pelvicwall or to the lower third of the vagina |
| IIA | Without parametrial invasion |
| IIA1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
| IIA2 | Clinically visible lesion >4 cm in greatest dimension |
| IIB | With obvious parametrial invasion |
| Stage III | The tumor extends to the pelvic wall and/or involves lower third of the vagina and/or causes hydronephrosis or non-functioning kidney |
| IIIA | Tumor involves lower third of the vagina, with no extension to the pelvicwall |
| IIIB | Extension to the pelvic wall and/or hydronephrosis or non-functioning kidney |
| Stage IV | The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. A bullous edema, as such, does not permit a case to be allotted to Stage IV |
| IVA | Spread of the growth to adjacent organs |
| IVB | Spread to distant organs All macroscopically visible lesions—even with superficial invasion—are allotted to stage IB carcinomas. Invasion is limited to a measured stromal invasion with amaximal depth of 5.00 mm and a horizontal extension of not >7.00 mm. Depth of invasion should not be >5.00mmtaken from the base of the epithelium of the original tissue—superficial or glandular. The depth of invasion should always be reported in mm, even in those cases with “early (minimal) stromal invasion” (~1 mm). The involvement of vascular/lymphatic spaces should not change the stage allotment. On rectal examination, there is no cancer-free space between the tumor and the pelvic wall. All cases with hydronephrosis or non-functioning kidney are included,unless they are known to be due to another cause. |
Treatment : Is decided based on the FIGO staging of the cervical cancer . (As described with the situation 2)
Standard Operative procedures
Inpatient :
Type I Hysterectomy with or without Salpingo oophorectomy
Trachelectomy
Type II / III Radical hysterectomy with or without Salpingo oophoprectomy &
Pelvic lymphadenectomy
Outpatient : Biopsy / ECC / Colposcopy / Diagnostic LEEP Cervix
Day Care : EUA / Cone Biopsy ./ LEEP Cervix ( Loop Eletric excision procedure) & Cystoscopy/ Sigmoidoscopy.
Referral Criteria :
Diagnosed cases of cervical cancer should preferably be referred to Regional Cancer Centre / Nearest Cancer centre / Hospital with facility of Radiation Therapy / Gynae Cancer Surgery.
Suspecious cases with diagnostic dilemma
Young patients with the diagnosis of early stage cervical cancer who opt for fertility preserving surgery.
Situation 2: At superspaeciality Facility in Metro location where higher – end technology is available.
Diagnostic criteria : are similar to that in Situation 1.
History
Complete Physical examination, Gynaecological examination including Per Vaginal & Per Rectal Examination.
Definitive Diagnosis
On histopathology of cervical growth biopsy / endocervical biopsy / Endocervical curettage / Cone Biopsy Cervix / Diagnostic LEEP Cervix.
Investigations
Histopathology / Pathologic review
Blood : Hb%, CBC, KFT, LFT, Blood Sugar F & PP, HbsAg, HIV
Imaging : X-ray Chest, CECT/ PET CT (Optional )/ MRI
EUA,Optional in stage IB2 and greater / doubtful parametrial involvement.
Cystoscopy /Sigmoidoscopy when bladder/ bowel involvement is suspected.
Other investigations required for the co- morbid conditions.
Cervical Cancer is staged as per the FIGO 2009 Criteria.
Treatment
PRIMARY TREATMENT DEPENDING ON THE CLINICAL STAGE OF THE DISEASE.
In early stage of the disease, stage IB & IIA similar cure rates are achieved with either primary surgery or radiation therapeutic treatment. The choice between the primary surgical or radiotherapeutic treatment depends on the age of the patient, co- morbid conditions, facilities & expertise available.(10)
Stage IA1
• Extrafascial hysterectomy
or
• Observe if patient desires fertility or if inoperable (11)
(only if cone biopsy has negative margins & no LVSI)
or
• Modified radical hysterectomy or trachelectomy
+ pelvic lymph node dissection if lymphovascular invasion
Or
ICRT when unfit for Surgery (12)
Dose 10,000 – 12,500 cGy at vaginal surface
Stage IA2
• Modified Radical hysterectomy (Type II ) +pelvic lymph node dissection
+/- para aortic lymph node sampling (13)
or
• Brachytherapy +/- pelvic RT(total point A dose : 75-80 Gy)
or
• Radical trachelectomy + pelvic lymph node dissection
+/- paraaortic lymph node sampling.(14)
Stage IB1 & IIA1
• Radical hysterectomy + pelvic lymph node dissection
+/- paraaortic lymph node sampling (category 1)(5)
or
• Pelvic RT + brachytherapy (total point A dose : 80-85Gy)
or
• Radical trahelectomy for tumors</= 2cm (Stage IB1)(14)
+pelvic lymph node dissection +/- paraaortic lymph node sampling.
Laproscopic Surgery: The role of minimal access surgery in management of cervical cancer is evolving at present. Presently, laparoscopic radical hysterectomy with pelvic lymphadenectomy can be offered to patients with stage IB1 cervical cancer as an alternative to the open abdominal radical hysterectomy in suitable patients with a low BMI and no major co‐morbid conditions. For optimizing results of the procedure, it should be done only by surgeons trained in the application of advanced laparoscopic surgery to gynecological cancer management and in specialized cancer centres with a large volume gynecologic oncological.
Stage IB2 & Stage IIA2
Treatment options
• Pelvic RT + concurrent cisplatin containing chemotherapy
+ brachytherapy (total point A dose >/= 85Gy( category 1)(15,16)
or
• Radical Hysterectomy + pelvic lymph node dissection
+ paraaortic lymph node sampling ( category 2B)
or
• Pelvic RT + concurrent cisplatin containing chemotherapy
+ brachytherapy (total point A dose 75-80Gy)
adjuvant hysterectomy (category 3)( 15)
Histopathology
Tumor size, type, Grade, Lymphovascular space involvement, involvement of vagina, microinvasion of the parametrium, Number of nodes dissected, Number of positive nodes. Involvement of the Endometrium/ tubes/ ovaries or any coexisting pathology.
ADJUVANT TREATMENT DEPENDING ON SURGICAL FINDINGS
- Negative Nodes
1. Pelvic RT if combination of high risk factors (category 1) (ie large primary tumor ,deep stromal invasion ,and/or lymphovascular space invasion)(17).
2. No above risk factors : Observe
➢ Positive Pelvic nodes and/or Positive surgical margin and /or Positive parametrium.
1. Pelvic RT + concurrent cisplatin containing chemotherapy
(category 1)(18)
+/- vaginal brachytherapy.
➢ Paraaortic lymph node positive by surgical staging
A. Chest CT / PET CT scan Negative
Paraaortic lymph node RT + concurrent cisplatin containing chemotherapy
+ Pelvic RT +/- brachytherapy.
B. Chest CT / PET CT Scan Positive for distant metastases
1. Suspicious Areas Biopsy Negative
• Paraaortic lymph node RT + concurrent cisplatin containing chemotherapy
+ Pelvic RT +/- brachytherapy.
2. Suspicious Areas Biopsy Positive
▪ Systemic therapy +/- individualized RT
PRIMARY TREATMENT DEPENDING ON THE CLINICAL STAGE
Stage IB2, Stage IIA2, Stage IIB, IIIA ,IIIB ,IVA
A. Radiological Imaging CT/ MRI / PET(19,20)
A1. Negative Adenopathy : Pelvic RT + concurrent cisplatin containing chemotherapy + brachytherapy.
A2. Positive Adenopathy : Consider needle Biopsy.
B. Surgical staging : Extraperitoneal or laparoscopic lymph node dissection (category 2 B)(21)
B1.Para aortic Nodes Negative : Pelvic RT + concurrent cisplatin containing chemotherapy (category 1)+ brachytherapy.
B2. Para aortic nodes Positive : See node status.
Stage IB2, Stage IIA2, Stage IIB, IIIA ,IIIB ,IVA Node Status
A. Pelvic lymph node positive & Paraaortic lymph node negative by surgical staging
Pelvic RT + concurrent cisplatin containing chemotherapy (category 1)+ brachytherapy.
B. Paraaortic lymph node positive by surgical staging.
B1. Further radiologic workup negative for distant metastases:
Pelvic RT + paraaortic lymph node RT +concurrent cisplatin containing chemotherapy + brachytherapy.
B2. Further radiologic workup positive for distant metastases:Consider Biopsy of suspicious areas.
If Biopsy Negative:
Pelvic RT + paraaortic lymph node RT + concurrent cisplatin containing chemotherapy + brachytherapy.
If Biopsy positive:
Systemic therapy +/- Individualized RT.
SURVEILLANCE
• Interval H& P.
• Cervical / vaginal cytology every 3-6 months for 2 yrs,then every 6 months for 3-5 yrs,then annually.
• Chest X Ray anually (optional)
• CBC, BUN, creatinine every 6 months (optional)
• PET CT scan as clinically indicated.
• Recommended use of vaginal dilator after RT.
• Patient education regarding symptoms.
Standard Operating Procedure
Inpatient : All major / radical surgical Procedures
Type I Hysterectomy with or without bilateral salpingo oophorectomy
Type II / Type III Radical Hysterectomy with or without salpingo
oophorectomy with Pelvic Lymphadenectomy.
Radical hysterectomy (type III) and bilateral pelvic lymphadenectomy involves removal of entire uterus, upper third vagina, bilateral parametria, uterosacral, utero‐vesical ligaments and bilateral pelvic lymph nodes. Bilateral salpino‐oophrectomy is discretionary.
Radical trachelectomy
Para aortic Lymphadenectomy / Sampling
Outpatient : Colposcopy Biopsy, ECC, Diagnostic LEEP Cervix.
Day Care : EUA & Cystoscopy, Rectosigmoidoscopy,Cone Biopsy
Referral Criteria :
On diagnosis of the cervical cancer on histopathology.
Young women with early stage ca cx opting for the fertility preserving surgery the patient
should be referred to the Gynae Oncology, Tertiary Cancer centre.
Guidelines by The Ministry of Health and Family Welfare :
Dr Anil K. D’ Cruz
Director and
Chief Head and Neck Services,
Tata Memorial Hospital, Mumbai

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd