- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
CABG has more AF,Stroke risk than PCI in LMCAD -EXCEL Trial
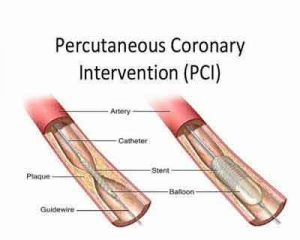
There is limited information on the incidence and prognostic impact of new-onset atrial fibrillation (NOAF) following the percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) for left main coronary artery disease (LMCAD).Dr.Ioanna Kosmidou and colleagues have found in The EXCEL Trial that New-onset atrial fibrillation (NOAF) occurred in 18 percent of patients undergoing coronary artery bypass grafting (CABG) but just in 0.1 percent of those receiving PCI.The results of the study have been published in Journal of the American College of Cardiology.
Kosmidou et al. studied 1,812 patients with left main coronary artery disease and no AFib at hospital presentation. They were all deemed fit for either CABG or PCI by a heart team and randomized to one of the procedures.In the EXCEL trial, 1,905 patients with LMCAD and low or intermediate SYNTAX scores were randomized to PCI with everolimus-eluting stents versus CABG. Outcomes were analyzed according to the development of NOAF during the initial hospitalization following revascularization.
They found that patients who developed NOAF within a few days of surgery were at a 3.02-fold risk of death and a 4.19-fold risk of suffering a stroke over the following three years. Compared to patients who didn’t develop atrial fibrillation (AFib) after CAGB, those who did had a higher 30-day risk of bleeding events and were more than twice as likely to meet the trial’s composite endpoint of death, heart attack or stroke within three years.
The authors suggested the extremely low rate of AFib in the PCI-treated group could be due to the relatively low-risk study population, few of whom presented with acute MI. They found older age, greater body mass index, and reduced left ventricular ejection fraction (LVEF) were independent predictors of NOAF in patients undergoing CABG.
The Researchers concluded that in patients with LMCAD undergoing revascularization in the EXCEL trial, new-onset atrial fibrillation, NOAF was common after CABG but extremely rare after PCI. The development of NOAF was strongly associated with subsequent death and stroke in CABG-treated patients. Further studies are warranted to determine whether prophylactic strategies to prevent or treat atrial fibrillation may improve prognosis in patients with LMCAD who are undergoing CABG.
For more details click on the link: https://doi.org/10.1016/j.jacc.2017.12.012

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd