- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
CABG best option of revascularization in diabetes
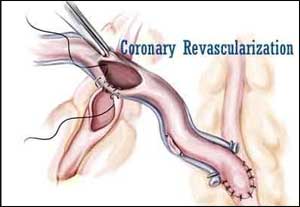
Dr.Krishnan Ramanathan, of University of British Columbia in Vancouver, Canada, and associates in a study assessed the he generalizability of the FREEDOM (Future REvascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multi-vessel Disease) trial in real-world practice among patients with diabetes mellitus and MV-CAD in residents of British Columbia, Canada by evaluating major cardiovascular outcomes in all patients with diabetes who underwent coronary revascularization between 2007 and 2014 (4,661 patients; 2,947 with ACS). The researchers found that in a real-world population of diabetic patients with Multi-Vessel -CAD, CABG was associated with a lower rate of long-term Major Adverse Cardiac and Cerebrovascular event (MACCE) relative to PCI for both acute coronary syndromes (ACS) and stable ischemic heart disease (SIHD).
The researchers in a large population-based database from British Columbia evaluated major cardiovascular outcomes in all diabetic patients who underwent coronary revascularization between 2007 and 2014 (n = 4,661, 2,947 patients with ACS).
They found that at 30 days after revascularization, the odds ratio for MACCE for ACS patients favored CABG (odds ratio, 0.49; 95 percent confidence interval [CI], 0.34 to 0.71), whereas, among patients with stable ischemic heart disease (SIHD), MACCE was not impacted by revascularization strategy (odds ratio, 1.46; 95 percent CI, 0.71 to 3.01; Pinteraction < 0.01). Over the longer term (median follow-up of 3.3 years), the benefit of CABG over PCI no longer varied by acuity of presentation (hazard ratio for MACCE in ACS and SIHD patients, 0.67 [95 percent CI, 0.55 to 0.81] and 0.55 [95 percent CI, 0.40 to 0.74], respectively; Pinteraction = 0.28).MACCE relative to PCI for both acute coronary syndromes, ACS and stable ischemic heart disease SIHD.
The authors concluded that in diabetic patients with MV-CAD, CABG was associated with a lower rate of long-term MACCE relative to PCI for both ACS and SIHD. A well-powered randomized trial of CABG versus PCI in the ACS population is warranted because these patients have been largely excluded from prior trials.
For further reference log on to :
http://www.onlinejacc.org/content/70/24/2995?sso=1&sso_redirect_count=1&access_token=

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd