- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Breast MRIs lead to more biopsies which detect fewer cancers : JAMA
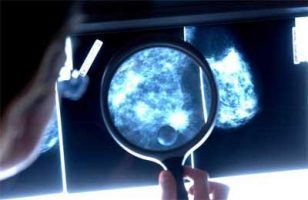
The standard screening test for Breast Cancer is a mammogram which may be performed as [per guidelines.Some women – because of their family history, a genetic tendency, or certain other factors – should be screened with MRIs along with mammograms.According to a U.S. study,women who get magnetic resonance imaging (MRI) screening tests for breast cancer are more likely to get invasive surgical biopsies to look for tumors than women who just get screening mammograms.In fact Breast MRIs lead to more biopsies which detect fewer cancers.These findings have been reported in JAMA Internal Medicine.
Doctors sometimes advise women with a prior breast cancer diagnosis or a genetic risk for certain aggressive, fast-growing tumors to get screening MRIs because these more detailed images may spot tumors sooner when malignancies are smaller and easier to treat. So it’s not surprising that the MRIs identified more spots that warranted follow-up testing with biopsies, said lead study author Diana Buist of the Kaiser Permanente Washington Health Research Institute in Seattle.
“But we had also expected that we would observe less invasive biopsies with more cancers detected,” Buist said by email. “Instead, after screening MRI we found more biopsies that were more invasive surgical and core biopsies, with lower cancer yield.”
Surgical or core biopsies involve removing large samples of tissue from the breast, and can result in scarring and infection. Fine-needle biopsies are less invasive, but may be more likely to miss abnormal tissue.
For the study, researchers examined data on 812,164 women who had screenings for breast cancer from 2003 to 2013.
Altogether, these women had a total of more than 2 million MRIs or mammograms during the study.
Women who had a personal history of breast cancer were more than twice as likely to get an invasive core or surgical biopsy after an MRI than after a mammogram, the study found. About 57 in 1,000 women got one of these invasive biopsies following an MRI, compared with 23 in 1,000 after a mammogram.
The difference was even more pronounced when women didn’t have a prior breast cancer diagnosis: 85 in 1,000 MRIs led to invasive biopsies compared with 15 in 1,000 mammograms.
Higher rates of benign abnormalities and lower rates of confirmed cancer cases were found with biopsies that followed MRIs than with those that followed mammograms, regardless of whether women had a personal history of breast cancer.
“These findings are concerning,” said Dr. JoAnn Elmore, a researcher at the David Geffen School of Medicine at the University of California, Los Angeles, who wasn’t involved in the study.
“Because screening involves healthy women, we do not want to introduce harm by our screening,” Elmore said by email. “Having more women undergoing breast biopsy without improving the cancer detection rate is a harm.”
The goal of screening is to detect tumors before they can be felt in a physical breast exam, catching cancer sooner when it’s easier to treat. Ideally, this should mean fewer women are diagnosed when tumors are bigger, rapidly growing and harder to attack.
A biopsy may be needed to test for cancer after a mammogram or MRI reveals abnormal cells or other signs that have the potential to represent malignant tisue.
The study wasn’t a controlled experiment designed to prove whether or how MRIs might lead to more invasive biopsies or fewer confirmed cancer cases.
“It is critical to understand that there is no medical test that is appropriate for everyone, and MRI is no exception,” said Dr. Richard Bleicher, a breast surgeon and professor at Fox Chase Cancer Center in Philadelphia.
“Some patients benefit from the sensitivity, but others will do just as well with mammography alone, and won’t suffer the consequences of all the false positives, unneeded biopsies and surgeries, and constant anxiety-producing follow-up and tests that could occur for months or years from false positives, which suggest that cancer is present when it is not,” Bleicher said by email.
For more details click on the link: SOURCE: bit.ly/2BvbXbq JAMA Internal Medicine

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd