- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Breakthrough!! Bioengineered vessel for dialysis evolve as patient's own blood vessel after implantation
A team of U.S based researchers developed a bioengineered blood vessel also known as the human acellular vessel (HAV) that recellularizes and evolve as patient's own blood vessel. The innovation appeared in Science Translational Medicine.
The investigational bioengineered blood vessel was generated by seeding human vascular cells into a biodegradable mesh scaffold within a bioreactor system. The vessel has been developed for as a hemodialysis conduit in patients with end-stage renal disease.
Conventional synthetic polymers and cadaveric human or animal tissues used in hemodialysis conduit are associated with several risks. Therefore, clinical demand for safe and effective vascular repair material is imperative.
The research team created a biodegradable mesh cylinder which was seeded it with human vascular cells and placed it in a bioreactor where culture media could be pulsed through it constantly. This system provided pulsatile distention, culture medium circulation, and facilitated decellularization of the resulting collagenous blood vessel (to remove all cells and immunogenic potential) while retaining the mechanical integrity of its extracellular matrix. The resulting acellular cylinders were placed in patients for various purposes (e.g., dialysis shunts).
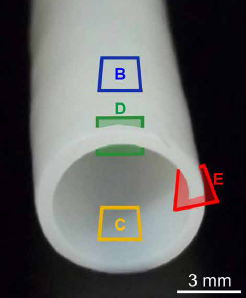
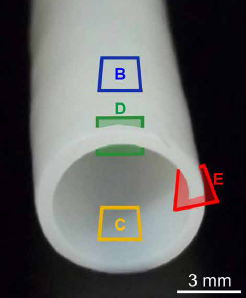 Image of a bioengineered HAV
Image of a bioengineered HAVThe researchers observed a substantial influx of alpha-smooth muscle actin–expressing cells into the HAV that progressively matured and circumferentially aligned in the wall of the bioengineered vessel. The bioengineered vessel was populated by the recipient's own immune identicals (some coming from adjacent soft tissue and some from blood) in the neoadventitia and later maintained by CD34−/CD31+ endothelial cells in the media and lumen of the HAV. Nestin+ progenitor cells differentiated into either alpha-smooth muscle cells or CD31 T cells that may contribute to early recellularization and self-repair of the HAV.
Based on their findings the researchers suggested that host myogenic, endothelial, and progenitor cell repopulation of HAVs transformed these previously acellular vessels into functional multilayered living tissues which are able to maintain blood transport and exhibit self-healing after cannulation injury, effectively rendering these vessels like the patient’s own blood vessel.
For more information, please click on the link

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd