- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Brain CT-ACR Practice Parameters 2015
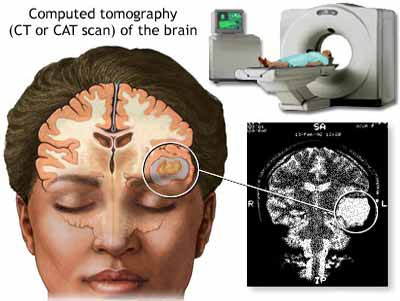
Computed tomography (CT) is utilized extensively in imaging of the brain. CT scanning provides more detailed information on head injuries, stroke, brain tumors and other brain diseases than regular radiographs (x-rays). CT of the brain is sufficient and diagnostic in many clinical circumstances such as in acute trauma, nontraumatic intracranial hemorrhage, evaluation of shunt malfunction, and selected postoperative follow-up. CT of the brain is a useful screening tool for indications such as acute mental status change, seizure, acute neurologic deficit, acute headache, and nonacute headache with neurologic findings. CT is useful as a screening modality for the presence of neoplasm and mass effect, particularly in conjunction with intravenous contrast.The ultimate judgement regarding the propriety of any specific procedure or course of action must be made by the practitioner in light of all the circumstances presented.
The American College of Radiology's Practice Parameter for the performance of Computed Tomography (CT) of the brain was revised in 2015.The ACR practice parameter is presented under the following sub-sections:
A. Indications
B. Specifics of the Examination
C.Equipment Specification
Indications for CT of the brain include, but are not limited to, the following:
1. Acute head trauma
2. Suspected acute intracranial hemorrhage
3. Vascular occlusive disease (acute and chronic) or vasculitis (including use of CT angiography and/or venography)
4. Aneurysm evaluation
5. Detection or evaluation of calcification
6. Immediate postoperative evaluation following surgical treatment of tumor, intracranial hemorrhage, or hemorrhagic lesions
7. Treated or untreated vascular lesions
8. Mental status change
9. Increased intracranial pressure
10. Headache
11. Acute neurologic deficits
12. Suspected intracranial infection
13. Suspected hydrocephalus
14. Certain congenital skull and brain lesions (such as, but not limited to, craniosynostosis, macrocephaly, and microcephaly)
15. Evaluating psychiatric disorders
16. Brain herniation
17. Suspected mass or tumor
18. CT guidance and image integration for neurosurgical, neurointerventional, and other therapeutic procedures
19. Certain skull lesions (such as, but not limited to, fibrous dysplasia, Paget disease, histiocytosis, osteolytic lesions, and skeletal tumors)
1. When MR imaging is unavailable or contraindicated, or if the supervising physician determines CT to be appropriate
2. Diplopia
3. Cranial nerve dysfunction
4. Seizures
5. Apnea
6. Syncope
7. Ataxia
8. Suspicion of neurodegenerative disease
9. Developmental delay
10. Neuroendocrine dysfunction
11. Drug toxicity
12. Congenital morphologic brain abnormalities
13. Abusive head trauma and postmortem forensic investigations
14. Brain death
15. Suspected shunt malfunctions or shunt revisions
The supervising physician must have complete understanding of the indications, risks, and benefits of the examination, as well as alternative imaging procedures. The physician should be familiar with relevant ancillary studies that the patient may have undergone. The physician performing CT interpretation must have a clear understanding and knowledge of the anatomy and pathophysiology relevant to the examination. The written or electronic request for CT of the brain should provide sufficient information to demonstrate the medical necessity of the examination and allow for its proper performance and interpretation.
Documentation that satisfies medical necessity includes
1) signs and symptoms and/or
2) relevant history (including known diagnoses).
Additional information regarding the specific reason for the examination or a provisional diagnosis would be helpful and may at times be needed to allow for the proper performance and interpretation of the examination. The request for the examination must be originated by a physician or other appropriately licensed health care provider. The accompanying clinical information should be provided by a physician or other appropriately licensed health care provider familiar with the patient’s clinical problem or question and consistent with the state’s scope of practice requirements.
A. General Consideration
CT protocols for brain imaging should be designed to answer the specific clinical question. The supervising physician should be familiar with the indications for each examination, relevant patient history, potential adverse reactions to contrast media, exposure factors, window and center settings, field of view, collimation, slice intervals, slice spacing (table increment) or pitch, dose reduction (eg, iterative reconstruction), and image reconstruction algorithms. Protocols should be reviewed and updated at least periodically to optimize the examination.
B. Brain Imaging
CT brain imaging may be performed with a sequential single-slice technique, multislice helical (spiral) protocol, or multidetector multislice algorithm . For CT of the brain, contiguous or overlapping axial slices should be acquired with a slice thickness of no greater than 5 mm. In the setting of trauma, images should be obtained and/or reviewed at window settings appropriate for demonstrating brain and bone abnormalities as well as small subdural hematomas or other sites of hemorrhage and soft-tissue lesions (subdural windows). For imaging of the cranial base, an axial slice thickness as thin as possible, but no greater than 3 mm with spiral techniques and 2 mm with multidetector and nonspiral techniques, should be used for 2-D reformatting or for 3-D reconstruction. Specially tailored protocols may also be considered, however, if clinical circumstances warrant, and under the direction of the supervising physician.
C. Contrast Studies
Certain indications require administration of intravenous (IV) contrast media or intrathecal contrast (eg, cisternography) during imaging of the brain. Intravenous contrast enhancement should be performed using appropriate injection protocols and in accordance with the ACR–SPR Practice Parameter for the Use of Intravascular Contrast Media . Cerebrospinal fluid (CSF) contrast administration requires the use of nonionic agents approved for intrathecal use and should be performed using appropriate protocols as outlined in the ACR–ASNR–SPR Practice Parameter for the Performance of Myelography and Cisternography.
D. Advanced Application
In addition to directly acquired axial images, reformatted images in coronal, sagittal, or other more complex planes may be constructed from the axial dataset to answer specific clinical questions, or the images may be manipulated to allow selective visualization of specific tissues such as in CT perfusion, CT volumetry, CT angiography/venography, multimodality image fusion, and mapping techniques. Such applications are better performed with helical, volume, or dual-energy datasets rather than routine axial sequential data. Also see the ACR–ASNR–SPR Practice Parameter for the Performance of Computed Tomography (CT) Perfusion in Neuroradiologic Imaging and the ACR–ASNR–SPR Practice Parameter for the Performance and Interpretation of Cervicocerebral Computed Tomography Angiography (CTA) .
EQUIPMENT SPECIFICATION
A. Performance Standards
To achieve acceptable clinical CT scans of the brain, the CT scanner should meet or exceed the following
specifications:
1. Scan times: per slice or image not more than 2 seconds
2. Slice thickness: minimum slice thickness 2 mm or less PRACTICE PARAMETER CT Brain / 5
3. Interscan delay: not more than 4 seconds (may be longer if intravascular contrast media is not used)
4. Limiting spatial resolution: must be measured to verify that it meets the unit manufacturer’s specifications. Limiting spatial resolution should be >10 lp/cm for a <24 cm display field of view (DFOV).
5. Table pitch: no greater than 2:1 for most CT scanners
6. For advanced applications (eg, perfusion imaging or CTA), cine-capable scanners are preferable with tube rotation ≤1 second and continuous cine imaging ≥60 seconds. See the ACR–ASNR–SPR Practice Parameter for the Performance of Computed Tomography (CT) Perfusion in Neuroradiologic Imaging.
B. Patient monitoring equipment and facilities for cardiopulmonary resuscitation, including vital signs monitoring equipment, support equipment, should be immediately available.
Appropriate emergency equipment and medications must be immediately available to treat adverse reactions associated with administered medications. The equipment and medications should be monitored for inventory and drug expiration dates on a regular basis. The equipment, medications, and other emergency support must also be appropriate for the range of ages or sizes in the patient populations.
Radiologists, technologists, and staff members should be able to assist with procedures, patient monitoring, and patient support. A written policy should be in place for dealing with emergencies such as cardiopulmonary arrest.
To read further read on the following link:
http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/CT_Brain.pdf
The American College of Radiology's Practice Parameter for the performance of Computed Tomography (CT) of the brain was revised in 2015.The ACR practice parameter is presented under the following sub-sections:
A. Indications
B. Specifics of the Examination
C.Equipment Specification
Indications for CT of the brain include, but are not limited to, the following:
A. Primary Indication
1. Acute head trauma
2. Suspected acute intracranial hemorrhage
3. Vascular occlusive disease (acute and chronic) or vasculitis (including use of CT angiography and/or venography)
4. Aneurysm evaluation
5. Detection or evaluation of calcification
6. Immediate postoperative evaluation following surgical treatment of tumor, intracranial hemorrhage, or hemorrhagic lesions
7. Treated or untreated vascular lesions
8. Mental status change
9. Increased intracranial pressure
10. Headache
11. Acute neurologic deficits
12. Suspected intracranial infection
13. Suspected hydrocephalus
14. Certain congenital skull and brain lesions (such as, but not limited to, craniosynostosis, macrocephaly, and microcephaly)
15. Evaluating psychiatric disorders
16. Brain herniation
17. Suspected mass or tumor
18. CT guidance and image integration for neurosurgical, neurointerventional, and other therapeutic procedures
19. Certain skull lesions (such as, but not limited to, fibrous dysplasia, Paget disease, histiocytosis, osteolytic lesions, and skeletal tumors)
B. Secondary Indications
1. When MR imaging is unavailable or contraindicated, or if the supervising physician determines CT to be appropriate
2. Diplopia
3. Cranial nerve dysfunction
4. Seizures
5. Apnea
6. Syncope
7. Ataxia
8. Suspicion of neurodegenerative disease
9. Developmental delay
10. Neuroendocrine dysfunction
11. Drug toxicity
12. Congenital morphologic brain abnormalities
13. Abusive head trauma and postmortem forensic investigations
14. Brain death
15. Suspected shunt malfunctions or shunt revisions
SPECIFICATION OF THE EXAMINATION
The supervising physician must have complete understanding of the indications, risks, and benefits of the examination, as well as alternative imaging procedures. The physician should be familiar with relevant ancillary studies that the patient may have undergone. The physician performing CT interpretation must have a clear understanding and knowledge of the anatomy and pathophysiology relevant to the examination. The written or electronic request for CT of the brain should provide sufficient information to demonstrate the medical necessity of the examination and allow for its proper performance and interpretation.
Documentation that satisfies medical necessity includes
1) signs and symptoms and/or
2) relevant history (including known diagnoses).
Additional information regarding the specific reason for the examination or a provisional diagnosis would be helpful and may at times be needed to allow for the proper performance and interpretation of the examination. The request for the examination must be originated by a physician or other appropriately licensed health care provider. The accompanying clinical information should be provided by a physician or other appropriately licensed health care provider familiar with the patient’s clinical problem or question and consistent with the state’s scope of practice requirements.
A. General Consideration
CT protocols for brain imaging should be designed to answer the specific clinical question. The supervising physician should be familiar with the indications for each examination, relevant patient history, potential adverse reactions to contrast media, exposure factors, window and center settings, field of view, collimation, slice intervals, slice spacing (table increment) or pitch, dose reduction (eg, iterative reconstruction), and image reconstruction algorithms. Protocols should be reviewed and updated at least periodically to optimize the examination.
B. Brain Imaging
CT brain imaging may be performed with a sequential single-slice technique, multislice helical (spiral) protocol, or multidetector multislice algorithm . For CT of the brain, contiguous or overlapping axial slices should be acquired with a slice thickness of no greater than 5 mm. In the setting of trauma, images should be obtained and/or reviewed at window settings appropriate for demonstrating brain and bone abnormalities as well as small subdural hematomas or other sites of hemorrhage and soft-tissue lesions (subdural windows). For imaging of the cranial base, an axial slice thickness as thin as possible, but no greater than 3 mm with spiral techniques and 2 mm with multidetector and nonspiral techniques, should be used for 2-D reformatting or for 3-D reconstruction. Specially tailored protocols may also be considered, however, if clinical circumstances warrant, and under the direction of the supervising physician.
C. Contrast Studies
Certain indications require administration of intravenous (IV) contrast media or intrathecal contrast (eg, cisternography) during imaging of the brain. Intravenous contrast enhancement should be performed using appropriate injection protocols and in accordance with the ACR–SPR Practice Parameter for the Use of Intravascular Contrast Media . Cerebrospinal fluid (CSF) contrast administration requires the use of nonionic agents approved for intrathecal use and should be performed using appropriate protocols as outlined in the ACR–ASNR–SPR Practice Parameter for the Performance of Myelography and Cisternography.
D. Advanced Application
In addition to directly acquired axial images, reformatted images in coronal, sagittal, or other more complex planes may be constructed from the axial dataset to answer specific clinical questions, or the images may be manipulated to allow selective visualization of specific tissues such as in CT perfusion, CT volumetry, CT angiography/venography, multimodality image fusion, and mapping techniques. Such applications are better performed with helical, volume, or dual-energy datasets rather than routine axial sequential data. Also see the ACR–ASNR–SPR Practice Parameter for the Performance of Computed Tomography (CT) Perfusion in Neuroradiologic Imaging and the ACR–ASNR–SPR Practice Parameter for the Performance and Interpretation of Cervicocerebral Computed Tomography Angiography (CTA) .
EQUIPMENT SPECIFICATION
A. Performance Standards
To achieve acceptable clinical CT scans of the brain, the CT scanner should meet or exceed the following
specifications:
1. Scan times: per slice or image not more than 2 seconds
2. Slice thickness: minimum slice thickness 2 mm or less PRACTICE PARAMETER CT Brain / 5
3. Interscan delay: not more than 4 seconds (may be longer if intravascular contrast media is not used)
4. Limiting spatial resolution: must be measured to verify that it meets the unit manufacturer’s specifications. Limiting spatial resolution should be >10 lp/cm for a <24 cm display field of view (DFOV).
5. Table pitch: no greater than 2:1 for most CT scanners
6. For advanced applications (eg, perfusion imaging or CTA), cine-capable scanners are preferable with tube rotation ≤1 second and continuous cine imaging ≥60 seconds. See the ACR–ASNR–SPR Practice Parameter for the Performance of Computed Tomography (CT) Perfusion in Neuroradiologic Imaging.
B. Patient monitoring equipment and facilities for cardiopulmonary resuscitation, including vital signs monitoring equipment, support equipment, should be immediately available.
Appropriate emergency equipment and medications must be immediately available to treat adverse reactions associated with administered medications. The equipment and medications should be monitored for inventory and drug expiration dates on a regular basis. The equipment, medications, and other emergency support must also be appropriate for the range of ages or sizes in the patient populations.
Radiologists, technologists, and staff members should be able to assist with procedures, patient monitoring, and patient support. A written policy should be in place for dealing with emergencies such as cardiopulmonary arrest.
To read further read on the following link:
http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/CT_Brain.pdf
brain tumorsComputed tomographyCT BrainCT Scanhead injuriesneoplasm and mass effectnonacute headachenontraumatic intracranial hemorrhagePractice Parametersseizurestroke
Source : American College of RadiologyNext Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd