- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Bariatric Surgery reverses hypogonadism, restores sex drive
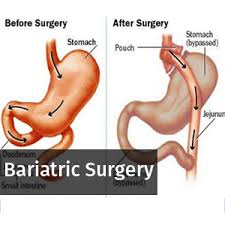
Weight loss resulting from a sleeve gastrectomy (obesity surgery) can facilitate the rapid reversal of obesity-related hypogonadism in morbidly obese men causing restoration of normal testosterone levels, according to a new research presented at 2018 European Congress on Obesity (ECO) in Vienna, Austria.
The study was conducted by Marco Rossato, a professor at the University of Padova, Italy, and colleagues to investigate levels of sex steroids immediately after rapid weight loss in a group of obese men who had undergone bariatric surgery, to determine how quickly those changes occurred.
Obesity in men is associated with hypogonadism; a condition characterized by insufficient production of testosterone and elevated estrogen levels. This is because of the interference caused by excess body fat in the metabolism of sex steroids leading to aromatization of androgens (such as testosterone) into estrogens within the adipose tissue itself.
The previous studies have evaluated the effects of weight loss on male hypogonadism a long time after the reduction in body fat has occurred, so it was not known how rapidly hormones began to return to normal in human subjects.
For the study, the researchers selected a group of 29 obese men with an average age of 40.5 years and an average body mass index (BMI) of 43.4kg/m2 (morbidly obese is defined as >40kg/m2). Blood tests were performed to measure total plasma testosterone, the sex hormones dihydrotestosterone (DHT), estradiol, luteinising hormone (LH), follicle-stimulating hormone (FSH), as well as sex hormone binding globulin (SHBG), prostatic-specific antigen (PSA), and leptin in subjects before and one month after they underwent a sleeve gastrectomy to reduce the size of the stomach. As a control, the team studied a group of 19 healthy age-matched, non-obese male subjects.
Key Findings:
- Among the obese subjects, 51.6% had hypogonadism and of those who had subnormal total testosterone, those with metabolic syndrome (45.2%) showed lower plasma testosterone than men without metabolic syndrome.
- BMI and waist circumference were found to be negatively correlated with total testosterone and plasma LH levels.
- Obese males had lower plasma testosterone than healthy subjects (10.8 vs. 15.7 nmol/L), higher estradiol levels (124.4 vs. 78.8 pmol/L), lower LH and FSH levels (3.6 and 2.5 vs 5.2 and 5.9 IU/L respectively).
- No differences were observed between the two groups in their DHT and PSA levels.
One month after the sleeve gastrectomy:
- Obese subjects showed a significant weight reduction, averaging 17.2 kg and the proportion with hypogonadism had fallen to 11.6%.
- Average testosterone levels increased by 85%, to a level greater than that observed in the healthy control group (18.9 vs 15.7 nmol/L).
- Estradiol levels fell by 35% while PSA levels rose by 70%.
The study demonstrates that while obese males show an elevated prevalence of hypogonadism, this is rapidly reversed (within one month) after significant weight loss following bariatric surgery. Testosterone levels are increased significantly while estradiol levels fall due to the rapid and significant loss of fat mass and the consequent decrease in aromatization of androgens to estrogens that typically occur in adipose tissue.
According to the authors, the clinical significance of the rapid increase in PSA plasma levels observed one month after bariatric surgery is still obscure and has to be confirmed on a larger number of subjects and after a longer period of observation after surgery and weight reduction maintenance.
They suggest that "it could be due to the rapid testosterone increase stimulating the prostate and/or to the rapid reduction in plasma volume after weight loss."
They say: "If you consider that obese males, as with all people with obesity, have higher prevalence of some type of cancer, including prostate cancer for men, this information could be of importance, since it could lead to doctors potentially missing cases of severe prostate disease in obese men."

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd