- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Bag-mask ventilation fails to improve on endotracheal intubation in cardiac arrest (CAAM)
Barcelona: Bag-mask ventilation fails to improve on endotracheal intubation in out-of-hospital cardiac arrest patients, according to late-breaking results from the CAAM trial presented in a Hot Line LBCT Session at ESC Congress.
“Sudden cardiac arrest is the main cause of death worldwide in previously healthy people,” said principal investigator Prof Frederic Adnet, an emergency physician at Avicenne Hospital in Bobigny, France. “Each year it causes 300 000 deaths in the US and more than 200 000 in Europe. Less than 10% of patients survive out-of-hospital cardiac arrest.”
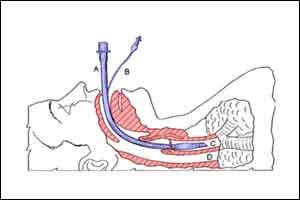
Airway management with endotracheal intubation has been the standard of care in cardiopulmonary resuscitation of out-of-hospital cardiac arrest victims. But its effectiveness has been challenged by retrospective studies from international registries which suggested that survival is much lower when ETI is performed during resuscitation. The studies have proposed that bag-mask ventilation is safer and more effective.
The CAAM trial was a prospective, randomised, controlled, multicentre trial which compared the impact of airway management with BMV versus ETI on survival with healthy brain function in out-of-hospital cardiac arrest patients.
The study included 2 043 out-of-hospital cardiac arrest patients from 15 centres in France and five in Belgium. Patients were randomised to receive BMV or ETI during cardiopulmonary resuscitation. The primary endpoint was survival with good neurological function, defined as Glasgow-Pittsburgh Cerebral Performance Categories (CPC) of 2 or less, at 28 days.
The investigators found the same rate of survival with good neurological outcome at day 28 in the two groups (4.2% with BMV versus 4.3% with ETI). However, the BMV technique failed in 6.7% of patients compared to 2.1% with ETI. There was a much greater incidence of regurgitation/aspiration with BMV (15.2%) compared to ETI (7.5%).
Prof Adnet said: “Bag-mask ventilation did not appear to be without danger in our trial. We were surprised by the much higher incidence of failure of the BMV technique compared with ETI. The higher incidence of regurgitation/aspiration in the BMV group confirms previous studies linking BMV with risks for the patient.”
He concluded: “BMV appears less safe than ETI as a means of ventilation during cardiopulmonary resuscitation in out-of-hospital cardiac arrest. Thus, we cannot recommend BMV as the standard method to ventilate out-of-hospital cardiac arrest patients during cardiopulmonary resuscitation.”

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd