- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
ASGE's recommendations for endoscopic eradication therapy in Barrett's esophagus
American Society for Gastrointestinal Endoscopy (ASGE) has released its new guideline on the use of endoscopic eradication therapy Barrett's esophagus.The new guideline has been published in the latest issue of journal GIE: Gastrointestinal Endoscopy.The guideline by the ASGE Standards of Practice Committee offers evidence-based recommendations and clinical guidelines addressing key issues related to Endoscopic Eradication Therapy (EET) in the management of Barrett's esophagus (BE)-related lesions.
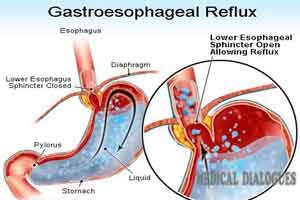
BE is a condition in which the normal lining of the esophagus develops abnormal lesions, sometimes due to chronic gastroesophageal reflux disease (GERD). It has been identified as a precursor to esophageal adenocarcinoma (EAC), a type of cancer that continues to become more common. In 2014, there were approximately 18,170 incident cases of esophageal cancer in the United States, nearly 60 percent of which were EAC. The outlook for patients with EAC has traditionally been poor.
Endoscopic eradication therapy (EET) has significantly changed the management of patients with BE-related lesions and allows a minimally invasive treatment approach that avoids the illness and deaths associated with the surgical procedure of esophagectomy (removal of some or most of the esophagus). Contemporary EET, supported by the published literature, entails endoscopic mucosal resection (EMR) of visible lesions within Barrett's segment and ablation (removal) techniques that include radiofrequency ablation (RFA) and cryotherapy.
Studies show that EET can result in complete removal of diseased tissue, leading to disease remission. This procedure is being performed not only at academic and tertiary care centers but also among community practices.
This document addresses EET vs. surveillance as an optimal management strategy for patients with dysplasia (abnormal growth of cells or tissue) and intramucosal EAC; comparison of EET with esophagectomy; the role of EMR and ablation; and recommendations for surveillance after achieving complete removal of lesions.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd